Three Cases of Local Anesthetic Systemic Toxicity following regional infiltration analgesia: The need for prompt recognition and treatment
Kevin A. S. Carroll*, Jonathan Henglein, Paul Boland, Paul Gallagher, Kermaan Mehta, Sabatino A. Leffe, Oktay Shuminov, Alejandro Betancourt-Ramirez, Shannon F. R. Small
Department of Surgery, South Shore University Hospital, Northwell Health, Long Island, New York, USA
Abstract
Introduction: The diagnosis and management of systemic toxicity in patients following regional infiltration analgesia is of paramount importance. While the mechanism and risk factors have been elucidated in previous studies, we believe that due to the potentially life-threatening nature of this rare occurrence, a greater focus on diagnostic precision and management enhancements is warranted.
Cases: Here, we describe three cases of LAST, the first in a 59 year old female following elective L4-L5 laminectomy and L5-S1 fusion, who suffered a cardiac arrest after receiving local Exparel and Marcaine at the time of closure; the second in a 69 year old woman following a rib block using local Exparel and Marcaine for the management of multiple rib fractures, who had a witnessed tonic-clonic seizure requiring intubation. The third patient is an 80-year-old male, who after an elective L4-L5 laminectomy and fusion, suffered a cardiac arrest after receiving local anesthetic (Exparel and Marcaine) at the time of closure. All patients were treated with intralipids and eventually recovered with no lasting deficits.
Conclusion: LAST events most commonly occur in the first minutes after injection, and are characterized by CNS and cardiovascular toxicities, as seen in these patients. Delayed presentations up to several days post exposure have been described. These cases exposed the opportunity for education in early recognition and most important, the need to improve the availability of intralipids. Prompt recognition and access to intralipid is critical to the treatment of LAST, and education regarding this rare but life-threatening condition is needed in surgical and trauma centers.
Introduction
Management of pain is a critical tool in both the post operative and trauma realms. With concerns for opioid addiction came the implementation of non-narcotic techniques to alleviate pain, specifically, the utilization of regional anesthetic agents. The instillation of local anesthetic agents as part of a multimodal approach to pain has been proven to reduce the use of narcotics9. Local anesthetic systemic toxicity (LAST) is a rare but well described potentially lethal event following the administration of a local anesthetic agent1.
Historically, local anesthesia was first documented to be used by dental surgeons6 for tooth extractions. Dr. William Halsted performed a peripheral nerve block by injecting cocaine in a patient’s exposed brachial plexus in 1884 with tremendous results6. Due to the toxic and addictive effects of cocaine, attention shifted to using a less toxic anesthetic agent. Procaine was first documented as being used in 1904 and was subsequently used for 40 years until Lidocaine, which was created in 1943 emerged6. This was a less addictive and less toxic anesthetic and has been used up to the present.
Local anesthetics can be classified as amino amides or amino esters which have different characteristics. Amino esters, such as benzocaine, chloroprocaine, cocaine, proparacaine and tetracaine are rapidly metabolized, less likely to result in systemic toxicity with a slow onset of action. Amino amides, such as articaine, bupivacaine, dibucaine, etidocaine, levobupivacaine, lidocaine, mepivacaine, prilocaine and ropivacaine are metabolized slowly, more likely to result in systemic toxicity, with a moderate to fast onset of action6. When looking at the types and dosing, we will refer to Table 1 and 2, this provides an overview of appropriate and maximum dosing which is important for practitioners utilizing local anesthetic agents.
Table 1: Local Anesthetic Agents and the appropriate dosing and maximum dosage
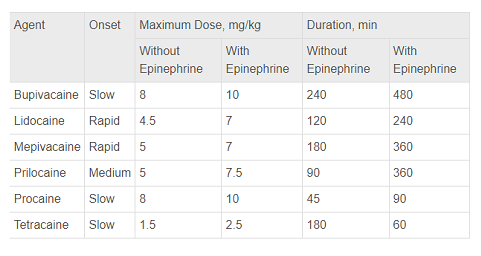
Reference: McLeod IK. Local anesthetics: introduction and history. Medscape. http://emedicine.medscape.com/article/873879-overview. Updated July 23, 2017. Accessed July 25, 2017.
Table 2: Additional Local Anesthetic Agents, appropriate dosing and maximum dosage
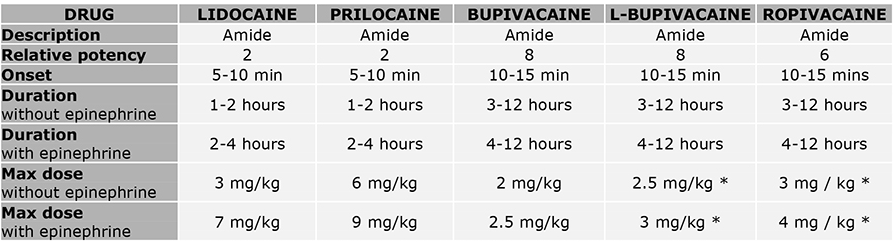
Reference: World Federation of Socieites of Anaesthesiologists. https://resources.wfsahq.org/atotw/pharmacology-for-regional-anaesthesia/. Accessed September 13, 2023.
The incidence of a LAST occurrence is currently estimated at 0.03%, or 0.27 episodes per 1,000 nerve blocks – a statistic that shows that while this may be an extremely rare ailment it is critical to recognize because it can be life threatening1. However, there is also a question of this syndrome being underdiagnosed due to the rare occurrence. Ongoing local anesthetic (LA) techniques, such as the fascial plane blocks and the use of tumescent anesthesia all increase the risk of LAST which raises future concerns and encourages increased awareness. When looking at the mechanism of how this adverse event occurs, there must be a focus on pharmacokinetics1,12,13. The toxicity is determined by rate of systemic absorption1. This is ultimately influenced by the perfusion of the site of injection. According to El-Boghdadly et al.; ‘LA agents exert their effect by attaching to the intracellular domain of the NaV channel, thereby inhibiting neuronal ion transfer and depolarization, and preventing neuronal transmission’1, therefore suppressing the nociceptive response. Increasing plasma concentrations of LA, which may be secondary to intravascular instillation of local anesthetic or decreased absorption, can affect excitatory pathways and therefore suppress neurological activity, resulting in altered mentation, loss of consciousness, coma and respiratory depression1. This can also result in disturbing cardiac conduction, resulting in myocardial dysfunction and loss of vascular tone. This can result in prolonged PR, QRS and ST intervals, resulting in both tachyarrhythmias and bradyarrhythmia's1. Central nervous system toxicity is the most common presentation of LAST. Other forms of presentation can be perioral paresthesia, confusion, visual disturbances, reduced consciousness as well as cardiovascular signs and symptoms such as palpitations, abnormal arrythmias and cardiac arrest1.
There are certain patient characteristics that can increase the risk of LAST syndrome. Increased weight/obesity, comorbidities such as chronic kidney disease, end stage renal disease and hepatic failure will result in decreasing the clearance rate of local anesthetics6. Geriatric trauma is a rising concern with the advancing age of the population, which unfortunately can increase the risk of LAST with the rising use of regional anesthesia.
Gitman et al. documented 47 occurrences of LAST between 2014 and 2016 with two deaths (4.3 percent). Only twenty-two patients were treated with intralipids (47 percent)7. Between 2017 to 2020 there were 36 cases of LAST reported in 34 peer-reviewed articles- notably 30 percent of the patients were greater than 65 years of age, with most events occurring in hospital (61%) and 17% in outpatient surgical centers8. Youth does not exempt patients from this disease process, as there was a documented case of a 33-year-old woman who suffered cardiac arrest two hours after liposuction of the thighs during which she received a total of 5000 mg of subcutaneous lidocaine8. 64% of patients received lipid emulsions in that cohort with two patients dying from anoxic brain injury8. It is important to mention that neonates and infants have a lower concentration of alpha 1 acid glycoprotein as compared to adults, which are bound to the local anesthetic agents14. This therefore increases the action of local anesthetic as they are unbound at higher doses, increasing the risk of systemic toxicity14.
The treatment of LAST is supportive care and intralipid use. Intralipid use was first described by Weinberg et al. in 1998, in which they demonstrated an improvement in bupivacaine induced cardiac arrest in rat models5,7. In 2010, The American Society of Regional Anesthesia and Pain Medicine recommended early use of intravenous lipid emulsion in the form of a bolus (1.5 ml/kg) followed by a continuous infusion (0.25 ml/kg/minute) up to 10 ml/kg in the first 30 minutes7. This case series will provide an overview of three patients who developed LAST after regional anesthesia.
Case Summaries
The first is a 59-year-old female with a past medical history of hypertension, hyperlipidemia, obesity and chronic back pain with radiculopathy who underwent an elective L4-L5 laminectomy as well as L5-S1 fusion. She underwent induction for elective intubation with Propofol and was maintained in a state of general anesthesia with infusions of Propofol and Remifentanil. A posterior lumbar region incision was made with an adjunctive local anesthetic of 20ml of 1% Lidocaine premixed with 1:100,000 Epinephrine. She remained stable without complications for over two hours. While still intubated and in the prone position, the surgical wound was then closed with additional local anesthetics of a premixed 13.3% Bupivacaine/Liposomal (Trade name Exparel) in a dose of 15ml, followed by a separate syringe of 15ml Bupivacaine 0.25%. Within several minutes the Anesthesia team noted sudden hypotension with a systolic blood pressure of 70 which was unresponsive to immediate IV fluid bolus, Phenylephrine 800mcg IVP (intravenous push) or Vasopressin 20 units IVP. The patient was then returned to a supine position and noted to have a wide complex arrhythmia alternating with a narrow complex and without a pulse. Cardiopulmonary resuscitation in accordance with the American Heart Association advanced cardiopulmonary life support (ACLS) protocol. The patient was given Epinephrine 1mg IVP without return of spontaneous circulation (ROSC). At this time LAST was suspected and she was then given 50ml of 20% Lipid emulsion resulting in ROSC but continued hypotension. An additional 50cc of 20% Lipids was then given as well as an intralipid infusion and a Norepinephrine infusion. Shortly after all vital signs improved, and the patient stabilized.
In the intensive care unit, care was coordinated along with toxicologists through the poison control center. Her lipid infusion was at 100cc/hr for two hours then discontinued. Her EKG revealed mild QTC Prolongation of 494ms. Official transthoracic echo revealed an ejection fraction of 65-70% with only grade 1 diastolic dysfunction. She had persistent mild hypotension and was transfused with two units of packed red blood cells. All laboratory findings improved over the next six hours and the patient was able to be safely extubated, awake and fully following commands. The patient eventually was discharged home with full recovery after about one week of working with physical therapy and further negative medical workup.
The second case is a 69-year-old female who was transferred to our level 2 trauma center from a community hospital after a ground-level fall, sustaining 4th through 7th displaced rib fractures on her right side with hemothorax and an occult pneumothorax. Her past medical history is significant for end-stage renal disease requiring hemodialysis, hypertension, hyperlipidemia, uterine cancer, status post hysterectomy in 2016 and 6 months of chemotherapy in 2017, and severe aortic insufficiency status post bioprosthetic aortic valve replacement in 2007. She was admitted to the Surgical Intensive Care Unit for pulmonary hygiene and multimodal pain control. Her multimodal pain regimen consisted of Acetaminophen, 4% lidocaine transdermal patch, gabapentin, and methocarbamol. A pain management consultation was called so she could be evaluated for regional anesthesia with the intent to limit narcotics and improve respiratory effort.
She was deemed appropriate for an erector spinae plane block and the pain management team proceeded in their standard fashion with 15mL of Bupivacaine/Liposomal and 15mL of Bupivacaine 0.25%. Aspiration prior to the injection of the local anesthetic was negative for air, blood, or CSF, and the local anesthetic spread was visualized under ultrasound guidance. However, upon completion of the nerve block, the patient was noted to have altered mental status. She was awake but not following commands and shortly thereafter developed a tonic-clonic seizure. Vital signs were initially normal, and she was intubated for airway protection. The patient then developed a widened QRS and became hypotensive. At this time the intralipid arrived at the bedside and she was bolused with 150mL of 20% Lipid emulsion and an infusion was initiated at 17mL/min. The patient never lost pulses and after approximately 750mL of the 20% lipid emulsion was administered, the patient returned to a sinus rhythm. Within four hours following the incident, the patient was weaned off norepinephrine, her serum lactate level went from 8mmol/L to 1.2 mmol/L, and she was successfully extubated. The toxicologist was called and agreed with the management and recommended supportive care thereafter. This patient ultimately required operative fixation of her rib fractures and evacuation of the hemothorax. She remained in the hospital for seven days after the rib fixation and was discharged to subacute rehabilitation.
The third case is an 80-year-old male, past medical history of hypertension, hyperlipidemia, coronary artery disease, history of coronary artery bypass grafting, type 2 diabetes mellitus, benign prostatic hyperplasia, human immunodeficiency virus, gastroesophageal reflux disease, orthostatic hypotension anxiety and depression, who was admitted to our hospital for an elective L4-L5 laminectomy and fusion for neurogenic claudication. As the surgical team was closing the surgical site, the patient was given 13.3% Bupivacaine/Liposomal 15ml followed by 15ml of Bupivacaine 0.25%. The patient then had an episode of bradycardia and concern for a possible seizure. The patient promptly became hypotensive- not responsive to a bolus of vasopressors. The patient was then turned back to the supine position and sustained a cardiac arrest. He underwent one round of CPR, and was given one push of epinephrine, with ROSC. The patient then received 150ml of 20% intralipid. He was started on multiple vasopressors to maintain hemodynamics. Cardiac anesthesia performed a Tracheoesophageal echocardiogram, which demonstrated inferior apical hypokinesis of the left ventricle. The patient was then transported to the surgical intensive care unit (SICU) on Propofol, Dobutamine and Norepinephrine. The patient was eventually extubated and was downgraded from the SICU to inpatient rehabilitation where he was eventually discharged.
All patients were treated with intralipids and eventually recovered with no lasting deficits. These patients did not have any delayed presentation of LAST syndrome despite this being a documented occurrence even up to several days.
Conclusion
LAST events most commonly occur in the first few minutes after injection, and are characterized by CNS and cardiovascular toxicities, as seen in all three of the patients presented here. Delayed presentations up to several days post exposure have been described1. These cases highlight the opportunity for education in early recognition and most importantly, the need to improve the availability of intralipids. It is hypothesized that intralipids work by a lipid sink and shuttle mechanism that results in absorption of highly lipid-soluble drugs within the lipid emulsion, resulting in removal from tissues affected by toxicity10. It is also thought that intralipids reverse cardiovascular collapse via reversing cardiac sodium channel blockade, reversing mitochondrial dysfunction and inhibiting the release of nitric oxide release producing an inotropic effect11. When looking at the amount of intralipids that should be given, a bolus of 1.5 ml/kg of 20% lipid emulsion and additional infusion of 0.25 ml/kg per minute should be infused2. This should continue for an additional ten minutes after obtaining hemodynamic stability. If the patient has not stabilized, there can be additional dosing of 0.5 ml/kg per minute with a maximum administered dose of 10 ml/kg for 30 minutes2. When looking at a stepwise approach to managing LAST, we recommend creating aids such as checklists or a treatment algorithm on all regional anesthesia carts (Figure 1). Oxygenation and ventilation with ACLS are priorities when there is concern for LAST. Lipid emulsion should also be given as described. Vasopressors should be given if correction of hemodynamics are not responsive to volume resuscitation. There should be avoidance of large doses of propofol, prioritize treating hypotension and bradycardia7.
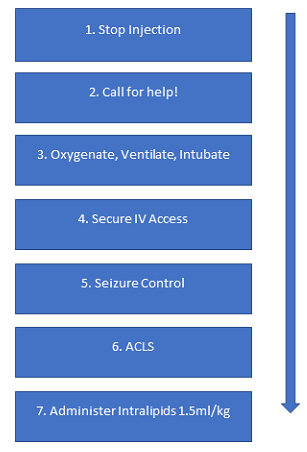
Figure 1:
Stepwise Approach to Management of LAST Syndrome
Reference: K. Carroll, MD, 2023.
A common agent given to these three patients was Exparel. There has been documentation of a highly disproportionate association with the use of Exparel and LAST3. Exparel has been found to prolong analgesia in wound beds up to an eight-fold increase in the length of time making it an ideal analgesic4, however there should be an awareness of this increased association, so that the clinician maintains a high index of suspicion for LAST.
With the increasing utilization of regional anesthesia, we suggest the following methods to prevent LAST syndrome: the continued use of ultrasound guidance, basic infiltration techniques such as avoidance of intravenous instillation, heightened awareness when performing regional anesthesia in patients with heart disease, extremes of age, increased frailty index and metabolic diseases such as end stage renal disease, chronic renal dysfunction and hepatic dysfunction5. As there is no known documented inclusion/exclusion criteria for regional anesthesia, providers should be aware of the patients clinical status, explore if patients has ever had concerns/complications with anesthetic agents and practice preventative measures to prevent these events such as ultrasound use and cardiac monitoring. Undertreatment could be related to underdiagnosis which demonstrates the need to educate providers at surgical and trauma centers to increase awareness and hopefully prevent poor outcomes.
This series alone has increased our institution’s awareness and prompted a quality initiative to implement the placement of intralipids on our procedural nerve block carts so that they are readily available. Our institution’s experience with these three patients has also resulted in the creation of an educational in-service to target the pain management team, emergency physicians and providers, surgical teams and the intensive care team. Prompt recognition and access to intralipid is critical to the treatment of LAST, and education regarding this rare but life-threatening condition is needed in surgical and trauma centers.
References
- El-Boghdadly K, Pawa A, Chin KJ. Local anesthetic systemic toxicity: current perspectives. Local Reg Anesth. 2018; 11: 35-44. doi: 10.2147/LRA.S154512. PMID: 30122981; PMCID: PMC6087022.
- Mahajan A, Derian A. Local Anesthetic Toxicity. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499964/
- Aggarwal N. Local anesthetics systemic toxicity association with exparel (bupivacaine liposome)- a pharmacovigilance evaluation. Expert Opin Drug Saf. 2018; 17(6): 581-587. doi: 10.1080/14740338.2017.1335304. Epub 2017 Jun 5. Erratum in: Expert Opin Drug Saf. 2018; 17(6): 655. PMID: 28538107.
- Grant GJ, Lax J, Susser L, et al. Wound infiltration with liposomal bupivacaine prolongs analgesia in rats. Acta Anaesthesiol Scand. 1997; 41(2): 204-7. doi: 10.1111/j.1399-6576.1997.tb04666.x. PMID: 9062600.
- Weinberg G. Systemic local anaesthetic toxicity: last and beyond Regional Anesthesia & Pain Medicine. 2019; 44: A33-A35
- Long B, Chavez S, Gottlieb M, et al. Local anesthetic systemic toxicity: A narrative review for emergency clinicians. Am J Emerg Med. 2022; 59: 42-48. doi: 10.1016/j.ajem.2022.06.017. Epub 2022 Jun 13. PMID: 35777259.
- Gitman M, Fettiplace M, Weinberg G, et al. Local Anesthetic Systemic Toxicity: A Narrative Literature Review and Clinical Update on Prevention, Diagnosis, and Management. Plastic and Reconstructive Surgery. 2019; 144(3): 783-795. doi: 10.1097/PRS.0000000000005989.
- Macfarlane AJR, Gitman M, Bornstein KJ, et al. Updates in our understanding of local anaesthetic systemic toxicity: a narrative review. Anaesthesia. 2021; 76: 27-39. https://doi.org/10.1111/anae.15282
- Chen YK, Boden KA, Schreiber KL. The role of regional anaesthesia and multimodal analgesia in the prevention of chronic postoperative pain: a narrative review. Anaesthesia. 2021; 76 Suppl 1(Suppl 1): 8-17. doi: 10.1111/anae.15256. PMID: 33426669; PMCID: PMC8369227.
- Ok SH, Hong JM, Lee SH, et al. Lipid Emulsion for Treating Local Anesthetic Systemic Toxicity. Int J Med Sci. 2018; 15(7): 713-722. doi: 10.7150/ijms.22643. PMID: 29910676; PMCID: PMC6001420.
- Lee SH, Sohn JT. Mechanisms underlying lipid emulsion resuscitation for drug toxicity: a narrative review. Korean J Anesthesiol. 2023; 76(3): 171-182. doi: 10.4097/kja.23031. Epub 2023 Jan 26. PMID: 36704816; PMCID: PMC10244607.
- Oda Y. Pharmacokinetics and systemic toxicity of local anesthetics in children. J Anesth. 2016; 30: 547-550. https://doi.org/10.1007/s00540-016-2201-6
- Liu Y, Zhang J, Yu P, et al. Mechanisms and Efficacy of Intravenous Lipid Emulsion Treatment for Systemic Toxicity From Local Anesthetics. Front Med. 2021; 8: 756866. doi: 10.3389/fmed.2021.756866
- Mazoit JX, Dalens BJ. Pharmacokinetics of local anaesthetics in infants and children. Clin Pharmacokinet. 2004; 43(1): 17-32. doi: 10.2165/00003088-200443010-00002. PMID:14715049
