Pericapsular Nerve Group Block in Hip Surgery: A Narrative Review
Daniela Bravo1, Rousmery Atton2,3, Diego Mora1, Julián Aliste1,3*
1Department of Anesthesiology and Perioperative Medicine, Hospital Clínico Universidad de Chile, University of Chile, Santiago, Chile
2Department of Anesthesiology, Pontificia Universidad Católica de Chile, Santiago, Chile
3Department of Anesthesiology, Clínica Las Condes, Santiago, Chile
Abstract
Study Objective: This narrative review discusses the anatomy, mechanism of action, techniques, indications and complications of the pericapsular nerve group block in a hip surgery setting.
Interventions: The MEDLINE, EMBASE and Google Scholar databases (inception to the first week of March 2023) were searched. For anatomy, mechanism of action, techniques, and complications, cadaveric research, randomized trials, retrospective studies and case series were considered. Nonetheless, for surgery indications, to highlight the best evidence available, only randomized trials without major discrepancies with their prospective registration, blinded assessment and sample size justification were retained for analysis.
Main Results: The anatomical studies suggest that pericapsular nerve group block may work through a combination of different mechanisms (i.e., blocking lateral capsule nerves, local anesthetic spread to the femoral nerve, spread towards medial capsule nerves). Compared to alternatives, except for the periarticular local anesthetic infiltration, pericapsular nerves group block results in similar or improved postoperative analgesia in total hip arthroplasty. It should be noted that the motor blockade has not been completely circumvented and the scarcity of adequate studies on other surgical procedures prevents from obtaining further conclusions about its indications.
Conclusions: The pericapsular nerve group block has become very popular after its first description as an analgesic motor-sparing technique for hip fractures. However, without an absolute motor-sparing effect, its current indication is better supported in postoperative analgesia for total hip arthroplasty. Therefore, further investigation is required to find the optimal motor-sparing analgesic block for hip surgery.
Abbreviations
AIIS= anteroinferior iliac spine; AON= accessory obturator nerve; FN= femoral nerve; FNB= femoral nerve block; IAI= intraarticular injection; IM= Iliacus muscle; ImM= iliacus minor muscle; IPE= iliopubic eminence; IPB= iliopsoas plane block; IPM= iliopsoas muscle; IPP iliopsoas plane=; IPT= iliopsoas tendon; LA= local anesthetic; LFCN= lateral femoral cutaneous nerve; ON= obturator nerve; PAI= periarticular local anesthetic infiltration; PACU= postanesthetic care unit; PeM= pectineus muscle; PENG= pericapsular nerve group; PMM= psoas major muscle; PPI= periportal local anesthetic infiltration; POD= postoperative day; RCT= randomized controlled trial; SIFIB= suprainguinal fascia iliaca block; THA = total hip arthroplasty; USG = ultrasound-guided; WI= wound local anesthetic infiltration.
Introduction
Major surgery of the hip, particularly arthroplasty and fracture repair, constitute increasingly common orthopedic procedures in an aging population. They often result in moderate to severe postoperative pain requiring multimodal analgesia. The relevance of this problem is such that it has become the focus of international societies efforts resulting in evidence-based guidelines for its management1,2. Periarticular local anesthesia infiltration (PAI) or peripheral nerve blocks are frequently included in perioperative analgesic protocols. Ideally, the latter should provide analgesia while minimizing motor block3, although lumbar plexus, fascia iliaca, and femoral nerve blocks are commonly performed for hip surgery, they inevitably result in motor weakness of the lower limb since they target the femoral nerve and the obturator nerve3,4.
In 2018, Giron-Arango et al. reported about the pericapsular nerve group (PENG) block for hip fracture, aiming to selectively cover the articular branches of the femoral nerve (FN) and accessory obturator nerve (AON) which would result in the sparing of the quadriceps and adductor muscles strength5. An additional early cadaveric study reports that the injectate could spread to the medial and inferior capsule, which are innervated by the articular branches of the obturator nerve (ON)6. Currently, the PENG block has been reported to provide analgesia for different types of hip procedures, particularly hip fracture fixation, total hip arthroplasty and hip arthroscopy. Anecdotal reports inform about other possible settings, but their analysis escapes the scope of this review7-10.
Despite its growing popularity, the PENG block is still not fully understood. After an initial description of a motor-sparing effect, some recent studies have reported quadriceps weakness after its use11-14, proposing local anesthetic (LA) spread towards the femoral nerve as the cause.
This review article aims to dissect published evidence focusing on relevant anatomic research, case series, retrospective studies and randomized clinical trials (RCTs) that have studied the PENG block, thereby offering readers a scope for benefits and the best indications for patients undergoing hip procedures.
Anatomy
Innervation relevant to hip surgical procedures
Both the lumbar and sacral plexuses participate in the innervation of the region. In broad terms, the acetabulofemoral joint is usually divided into its anterior and posterior components, the former innervated by articular branches from the FN, ON and AON, while the posterior aspect is provided by the nerve to quadratus femoris, sciatic and superior gluteal nerves15,16.
The skin supply of the anterior hip region arises from the iliohypogastric nerve, genitofemoral nerve, and FN17. Nonetheless, the posterolateral area is the one involved in the incisions of most hip surgeries, receiving its cutaneous innervation from the superior cluneal, subcostal, iliohypogastric and lateral femoral cutaneous nerves18.
Anatomical characteristics relevant for the PENG block
At the level where PENG block is performed, in between the anteroinferior iliac spine (AIIS) and the iliopubic eminence (IPE), several muscular, fascial, and neurovascular structures can be found. The muscular components include (from lateral to medial) the iliacus minor muscle (ImM), the iliacus muscle (IM) and the psoas major muscle (PMM). Additionally, the iliopsoas tendon (IPT), a conjoined tendon fused by the lateral PMM tendon and the medial iliacus tendon, is in the depth of this muscular complex and lateral to the IPE19. At this point, the fascia iliaca wraps all these muscular elements and, its thickened anteromedial portion which attaches inferomedially to the IPE, the iliopectineal fascia, separates them from the femoral vessels and the pectineus muscle (PeM)20. The iliopectineal bursa lies deep to the IPT, with its proximal end lying on the IPE and distally passing anteriorly to the capsule as it extends towards the lesser trochanter19. The FN and the femoral branch of the genitofemoral nerve can be seen in this anatomic section; the former in the anterior surface of the iliopsoas muscle (IPM), and the latter adjacent to the femoral vessels17.
Considering that the highest concentration of nociceptive fibers is located in the anterior and superolateral hip joint capsule, in contrast with mechanoreceptors with no nociceptive fibers in the posterior region21, special attention has been given to the origin and pathway of the articular branches originated in the lumbar plexus as a target of selective regional blocks for analgesia after hip surgical procedures.
The FN descends from its origin passing laterally through the PMM to be positioned on a groove formed between the IM and PMM as it moves caudally towards the inguinal ligament. The articular branches from the FN will innervate all four anterior quadrants to the hip capsule and mostly arise proximal to the inguinal ligament (high branches) and deepen into the thickness of the IM to reach the periosteal surface of the pubis in an area between the AIIS and the IPE as they travel caudally to the joint16. Low branches either pierce the IM or move inferiorly and then recur to innervate the hip capsule16,22.
The ON descends on the deep medial aspect of the PMM. The articular branches of this nerve will innervate the inferomedial and inferolateral hip capsule16 and may arise before entering or within the obturator canal on its path to leave the pelvis (high branches). Alternatively, these branches can arise once the ON has divided into its anterior and posterior components (low branches). These small nerves are located in the sub pectineal plane and course over the inferomedial acetabulum16.
The presence of the AON ranges between 8-54%16. When found, this nerve initially travels with the ON, but as it moves caudally, the AON passes directly anterior to the IPE, deep to the PeM, giving off branches that will consistently innervate the medial capsule15,16.
Consequently, the three aforementioned nerves seem to be the primary transmitters of pain in the hip joint. A recent anatomical study suggests a higher incidence of AON presence than previously reported (53% versus 8-33%)16. Additionally, this trial revised the pattern of sensory distribution of the nerves to the anterior hip capsule, giving preponderance to the high branches of the FN and the AON16 (Figure 1). However, other cadaveric studies have found a greater relevance of the FN low branches and lower frequency of the AON23. Nevertheless, these findings shouldn’t be considered contradictory since they involve small sample sizes and (probably) different ethnic origins of the cadavers.
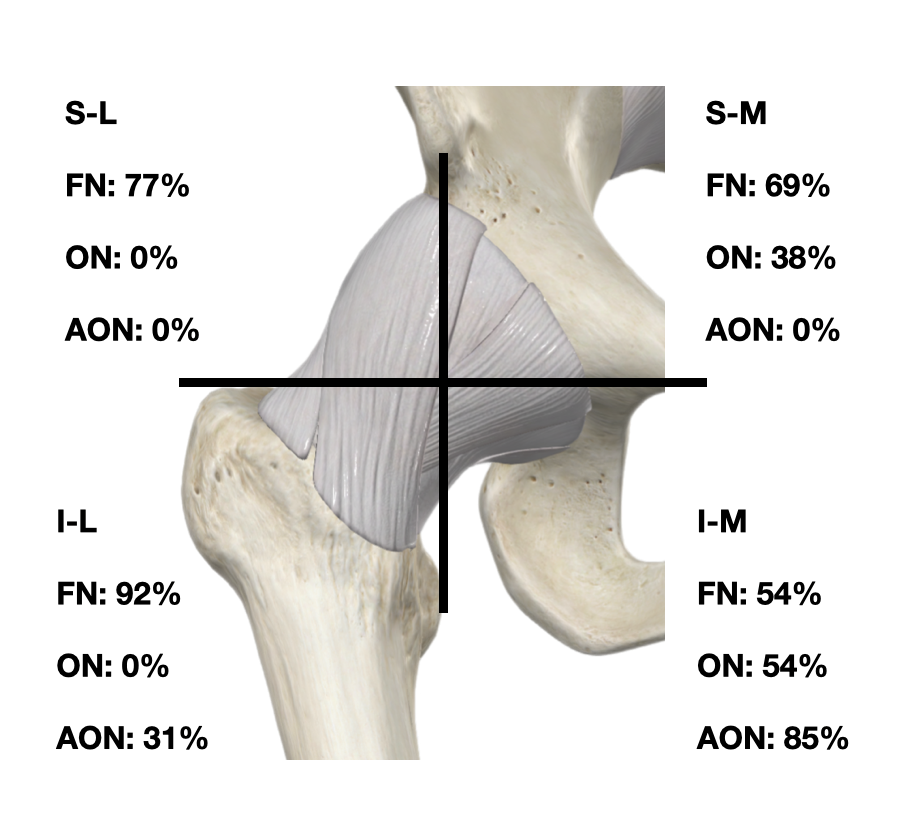
Figure 1: Frequency of contribution by nerve to the anterior quadrants of the hip capsule.
S-L: superolateral, S-M: superomedial, I-L: inferolateral, I-M: inferomedial, FN: femoral nerve, ON: obturator nerve, AON: accessory obturator nerve. Data obtained from Table 3 of Short et al.16
Technical aspects of PENG Block
Increasingly popular for its simplicity, security and effectiveness, the technique underlying the PENG block5 can be divided into two separate components: 1) identification of the injection site, and 2) needle tip position / LA injection in the plane between the IPM and the iliac bone.
Identification of injection site
The PENG block was described as an ultrasound-guided single injection of LA targeting the musculofascial plane between the pubic ramus and the IPT5. Most commonly, the block is performed with the patient in the supine position, although anecdotal reports have described it in lithotomy position for urologic procedures8 and also with a 90° hip abduction in the pediatric population24.
Predominantly, a curvilinear low-frequency ultrasound probe is used due to the wider field of vision and the depth of the target in the average adult population. However, the use of a linear high-frequency probe (8-13MHz), especially for thin or young patients, has been reported as well24-26.
After adequate skin disinfection, the selected probe is placed in a transverse position over the AIIS. Then, it is aligned with the pubic ramus by a 30-45º degrees rotation, clockwise or counterclockwise, depending on the side5. Alternatively, other authors first prefer to recognize the hip joint in a transverse section, and then move the probe cranially until the IPE and AIIS are visualized (Figure 2a) by achieving the alignment through slight probe rotation27.
Besides ultrasound guidance (USG), the PENG block can also be performed through anatomical landmarks28 and fluoroscopy, more frequently in the setting of chronic pain management29. No RCT has compared the three modalities. However, the landmark technique, with its blind needle insertion, has been criticized for the inherent possibility of vascular puncture and subsequent risks of hematoma and/or systemic local anesthetic toxicity28. Furthermore, although theoretically better than surface landmarks, but hindered by its unavailability in most operative settings, fluoroscopy might not be exempt from the previously described risks. Moreover, fluoroscopy adds radiation/contrast exposure without accurately certifying the injection plane.
A recent cadaveric study by Kitcharanant et al.23 described a surgeon-performed PENG block for total hip arthroplasty (THA) with an anterior approach under direct vision, where no signs of intramuscular injection were observed while performing the blocks.
In summary, until adequate RCTs define the optimal technique for the PENG block musculofascial plane identification, we suggest anesthesiologists favor USG instead of surface landmarks or fluoroscopy.
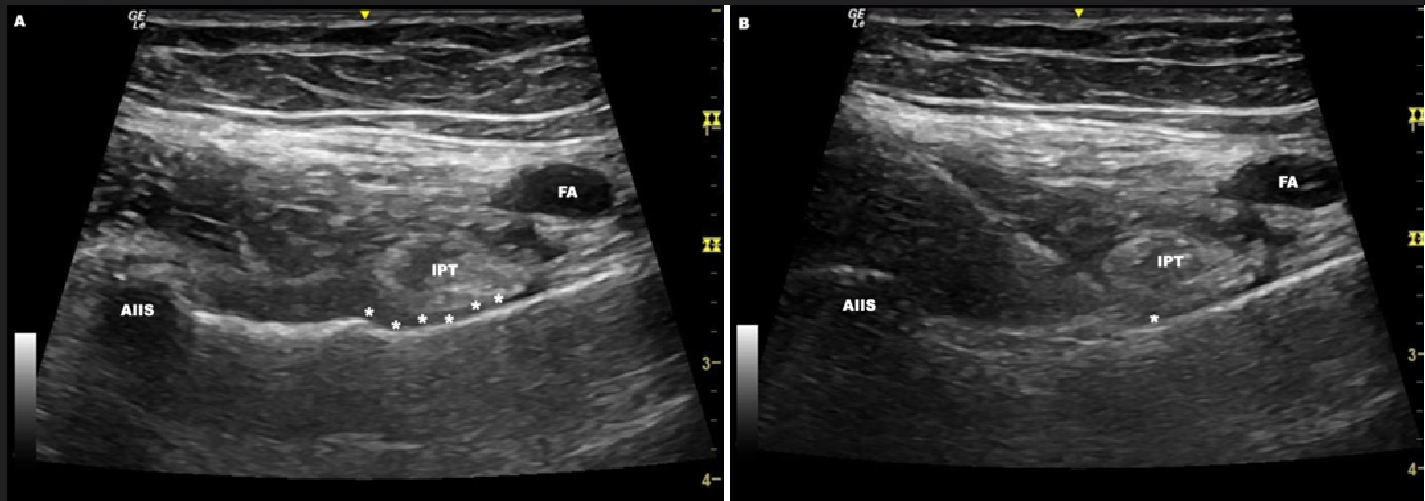
Figure 2: A) Ultrasonographic target in the PENG block. B) Ultrasonographic view of the needle insertion in the PENG block.
AIIS= anteroinferior iliac spine; FA= femoral artery; IPT= iliopsoas tendon.; asterisks= iliopsoas plane; asterisk= needle tip
Needle tip positioning/Local Anesthetic Injection
After proper anatomical identification, a block needle is introduced under USG from lateral to medial in an in-plane approach to reach the aforementioned musculofascial plane5. The target is the bony structure between the AIIS and the IPE, deep to the IPT (Figure 2b). This plane continues with the hip pericapsular plane6.
Once the needle tip has been positioned, the LA solution is injected, aiming for a linear spread above the bone surface. As in other fascial plane blocks, the correct spread can be confirmed with small aliquots of normal saline solution to avoid wasting the anesthetic injectate in the wrong spot. After the initial reports of quadriceps motor compromise, the authors of the approach have provided additional tips to make sure that the desired plane has been achieved by piercing the fascia (i.e., to make rotational movements of the needle once the bone has been contacted), advocating the mechanism of the FN coverage by intramuscular deposition of LA30 or to avoid a too medial injection site, which could result in migration of LA through the intermuscular plane between the PeM and IPM31. Additionally, an alert of the high-volume effect was provided31.
In summary, further investigation is required to determine the most efficient way of identifying the predefined injection site, the ideal injection site (if just one) and unequivocal ultrasonographic signs of block success while maintaining its motor-sparing purpose.
Mechanism of Action of PENG Block
The mechanism of action for the PENG block relies on the injectate spread of the injected solution in the plane between the IPM and the anteromedial hip capsule. This place for deposition of LA aims to selectively block the articular branches of the FN (high branches) and the AON5. However, the original clinical series of Giron-Arango et al.3 left uncertainty regarding the ability of the injectate to reach the articular branches of the ON as they pass in the subpectineal plane (between the pectineus and obturator externus muscles). In a subsequent cadaveric exploration using dye injectate, the spread showed that the entire anterior hip joint capsule was stained, with 10 and 20mL, suggesting that the low branches from the FN and the twigs from the ON could be also covered6. Some authors hypothesized that the LA could spread through the lacuna musculorum and reach the subpectineal plane by following the ilioinfratrochanteric muscular bundle below the IPT32. However, the articular branches from the obturator nerve would require a subpectineal plane injection to be covered since the iliopectineal bursa obstructs the spread of injectate towards the obturator nerve33.
In the following years, several reports9,25 and RCTs (that assessed sensory-motor function of the thigh)11-14 have raised the alert of a more extensive spread where LA could advance ventrally toward the FN. The postulated mechanisms for this effect can be separated into; 1) an inadequate deposition of the LA or, 2) the use of a large volume that results in extensive hydro-dissection. In the first scenario, either frank intramuscular or unnoticed injection between de IM and its fascia could result in this clinical finding25,31. Additionally, advancing the needle too medially in relation to the IPT could also result in a spread through the intermuscular plane between the PeM and PMM31. On the other hand, the effect of volume can be seen in the very first cadaveric report, where dye spread reaches the FN with 20mL6, a finding that has been clinically enhanced using 30mL9. Other mechanisms can be encountered in the literature, such as LA tracking back along the high branches toward the FN34 or even the piercing (and rupture) of the iliopectineal bursa can result in injection outside the iliopsoas plane, allowing the LA solution to migrate anteromedially or intraarticularly19. However, these are theories awaiting confirmation.
A PubMed database search (inception until the first week of March 2023) looking for anatomical studies of the PENG block investigating the mechanism of action resulted in three articles in correspondence form and two original research papers6,23,35-37. Their characteristics and main findings are listed in Table 1. Besides the obvious scarcity of studies, it becomes evident that elements such as injected volume, underlying pathology (i.e., fracture, arthrosis, etc.), surgical approach and timing (pre, intra or post-surgery) may play a relevant role in the pattern of diffusion and, consequently, in the resulting block of the different nerve branches.
Table 1: Anatomical studies investigating mechanism of action of PENG block.
|
Authors (year) |
Cadavers/ PENG blocks (n) |
Type of cadaver |
Technique |
Contrast or dye injectate |
Imaging vs. dissection |
Covered area (if described) |
FN articular branches |
ON |
AON articular branches |
Comments |
|
Tran 20196 |
1 / 2 |
Lightly embalmed |
US-guided |
10 and 20mL of methylene blue |
Dissection |
Both injections spread in the defined bursal space between the IPM and anterior hip joint capsule |
Likely, but not dissected |
Likely, but not dissected |
Likely, but not dissected |
With 20mL both the FN and ON main nerves are stained. |
|
Altinpulluk 202035 |
5 / 10
1/1 (prosthetic hip joint) |
Not stated |
Fluoroscopy-guided |
10mL of contrast + Sequence of injections: 51015 20mL |
Fluoroscopy |
Cranially under the IPM and caudally in the valley between the iliofemoral ligaments laterally, the pubofemoral ligament medially and the IPT and bursa anteriorly and extending down to its insertion on the lesser trochanter.
Spread was limited to superior border of the acetabulum. No diffusion occurred with increase in volume. Contrast reached the margin of the IPE. |
NA |
NA |
NA |
|
|
Ciftci 202136 |
1 / 2 |
Unembalmed |
US-guided |
20 and 30mL of 0.25% methylene blue |
Dissection |
There was dye spread below the tensor fascia lata with the 20 ml volume. There was dye spread throughout iliopsoas, around the vastus medialis, and gluteus medius muscles with the 30 ml volume |
Not dissected |
Not dissected |
Not dissected |
There was spread of dye around the FN.
In the 30mL group, there was dye spread around the FN trace from inguinal to the knee, around the LFCN, and ON. |
|
Kitcharanant 202223 |
11 / 18 |
Unembalmed |
Performed by surgeon under direct vision |
20 mL of 0.1% methyleneblue |
Dissection |
There’s no direct description of the covered area by methylene blue, however, nerves and branches are thoroughly addressed. |
Stained (100% cases)
(High branches were found in 2 cases) |
Stained
(Found in 3 cases) |
Stained
(Found in 2 cases) |
FN was stained in 1 case and ON in 2 cases. LFCN wasn’t stained. |
|
Kim 202337 |
18 / 36 |
Unembalmed |
US-guided |
10, 20, or 30 mL of a 200mL solution composed by distilled water, latex solution cobalt blue ink and standard barium in a 140:40:1:20 ratio. |
Computed tomography and dissection |
Cephalad-lateral spread is dominant and volume dependent.
Intramuscular uptake was most extensive and prominent in the 30mL specimens. |
Stained with 20 and 30mL. |
Stained with 20 and 30mL.
(Found in 9% of cases; one on each group)
|
Rarely stained.
(1/12 10mL, 2/12 20mL, 1/12 30mL) |
FN showed volume dependent staining.
(4/12 10mL, 8/12 20mL 10/12 30mL).
From figures, it seems that the staining capacity of the injected dye is not as marked as other solutions. |
AON: accessory obturator nerve, FN: femoral nerve, IPE: iliopectineal eminence, IPM: iliopsoas muscle, IPT: iliopsoas tendon, LFCN= lateral femoral cutaneous nerve, NA: not applicable, ON: obturator nerve
From a pharmacological standpoint, PENG block has been performed using long-acting LA like bupivacaine and ropivacaine but in different concentrations11-14,38,39 and in a few experiences with adrenalized mixtures12-14. Although adjuvants have been described5,25, there is no properly registered or designed trial that has studied the role of different LAs, different LA concentrations, and adjuvant addition (types, doses, or mixtures) in the analgesic or motor-sparing performance of this block. Furthermore, after Girón-Arango et al.5 first report using an arbitrary volume of 20 mL, no dose-finding study or RCT has looked for or compared volumes/concentrations of LAs.
In summary, the combined literature findings suggest that the PENG block mechanism of action is the result of the blockade of the articular branches of the FN and AON, being the ON branches reached only in a volume-dependent manner, and when at least 20mL are used. This approach can result in LA migration towards the FN and ON main trunks; however, its occurrence may depend on factors such as volume of injectate and possible deviations from the original technique. Anatomical studies of the PENG block are still very limited and heterogeneous. Additionally, future research is granted to elucidate pharmacological aspects of the block, particularly for the setting of enhanced recovery after hip surgery.
Indication of PENG Block
The PENG block has been reported in different hip procedures in adult and pediatric patients. However, to avoid biased anecdotal findings, this section includes the results derived from RCTs comparing PENG block to sham/no block/other blocks. We chose to exclude all RCTs without proper prospective trial registration or major discrepancies between registered and reported protocols. Additionally, properly registered trials without blinded assessment or sample size justification were also discarded in order to provide readers with the highest quality evidence available40. The bibliography of all retained references was also hand-searched for additional RCTs. The co-authors (DB-RA-DM-JA) conducted the final literature search using the MEDLINE, EMBASE and Google Scholar databases (inception until the first week of March 2023).
The term "Pericapsular nerve group block" was queried and yielded a total of 26 RCTs comparing the PENG block to sham/no block/other blocks. A total of seven RCTs were kept for analysis (Table 2)11-14,38,39,41. Regretfully, the majority19 of trials lacked sample size justification, blinded assessment, proper registration or displayed serious discrepancies between registered and reported protocols. For the sake of completeness, these discarded studies (and the reason for their exclusion) are presented in Appendix 141-60.
Table 2: Randomized trials comparing PENG block.
|
Authors (year) |
N |
Surgery |
Study group |
Control group |
Quadriceps assessment |
Findings Primary Outcome |
Comments |
|
Pascarella (2021)38 |
60 |
THA |
Preoperative PENGB (20ml 0.375% Ropivacaine) + postoperative WI (20ml 0.375% Ropivacaine) |
Postoperative WI (20ml 0.375% Ropivacaine) |
None |
The maximum pain score in PENGB was significantly lower than in the control group at all time-points. |
Faster rehabilitation without differences in LOS |
|
Aliste (2021)12 |
40 |
THA |
Postoperative PENGB (20ml adrenalized 0.5% Bupivacaine) |
Postoperative SIFIB (40ml adrenalized 0.25% Bupivacaine) |
Qualitative: preop, 3hrs, 6hrs, 24hrs |
PENGB resulted in a lower incidence of quadriceps motor block at 3hrs and 6hrs |
No differences in secondary outcomes. Motor block in PENGB at 3 and 6 hrs |
|
Zheng (2022)41 |
71 |
THA |
Preoperative PENGB (20ml 0.5% Ropivacaine) + postoperative IAI (20ml 0.5% Ropivacaine) |
Postoperative IAI (20ml 0.5% Ropivacaine) |
Quantitative: preop, 6hrs, 24hrs, 48hrs |
PENGB decreased the highest pain just in PACU. |
Included fracture patients. Decreased postoperative quadriceps strength in both groups. |
|
Choi (2022)13 |
58 |
THA |
Preoperative PENGB (20ml adrenalized 0.2% Ropivacaine) |
Preoperative SIFIB (30ml adrenalized 0.2% Ropivacaine) |
Quantitative: preop, 6hrs, 24hrs, 36hrs |
PENGB just lowered pain scores at rest in t at 6hrs and 24hrs |
No differences in other outcomes including motor block, present in both groups. |
|
Bravo (2023)14 |
60 |
THA |
Postoperative PENGB (20ml adrenalized 0.5% Bupivacaine) |
Postoperative PAI (60ml adrenalized 0.25% Bupivacaine) |
Qualitative: preop, 3hrs, 6hrs, 24hrs |
No differences in postoperative quadriceps block |
PAI had better postoperative analgesia but also induced postoperative quadriceps weakness |
|
Lin (2021)11 |
60 |
HFS |
Preoperative PENGB (20ml 0.75% Ropivacaine) |
Preoperative FNB (20ml 0.75% Ropivacaine) |
Qualitative: PACU, POD1 |
PENGB experienced less pain in POD0 |
Mixed cohorts of intra- and extra capsular fractures and different types of surgeries |
|
Amato (2022)39 |
70 |
HA |
Preoperative PENGB (20ml 0.5% Ropivacaine) + Postoperative PPI (30ml 0.25% Bupivacaine) |
Postoperative PPI (30ml 0.25% Bupivacaine) |
None |
No differences in postoperative pain |
Both groups reported moderate to severe pain. |
THA= total hip arthroplasty; HFS= hip fracture surgery; HA= hip arthroscopy; PENGB= pericapsular nerve group block; WI= wound infiltration; LOS= length of stay; SIFIB= suprainguinal fascia iliaca block; IAI= intraarticular local anesthetic injection; PACU= postanesthetic care unit; PAI= periarticular local anesthetic infiltration; FNB= femoral nerve block; POD= postoperative day; PPI= periportal local anesthetic infiltration
The Cochrane Database Tool to assess the risk of bias was applied to the selected RCTs. The domains evaluated included: the adequacy of sequence generation; allocation concealment; blinding; how incomplete outcome data was addressed; selective outcome reporting; and other sources of bias (i.e., study design issues, early trial termination, baseline imbalance in study groups). Thereafter, domains were categorized as "yes" (green i.e., low risk of bias) "no" (red i.e., high risk of bias) and "unclear" (yellow i.e., unknown risk of bias) (Figure 3).
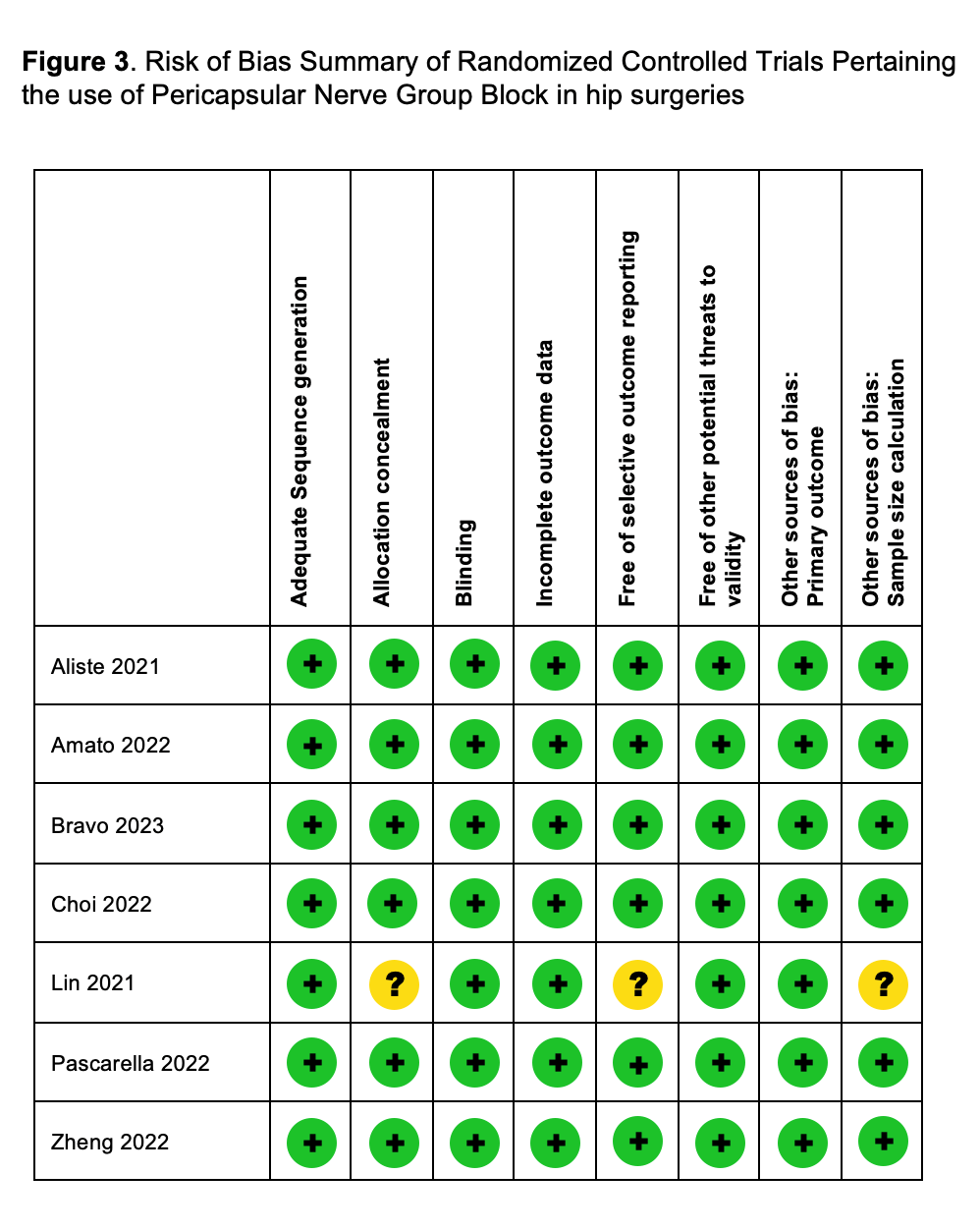
Figure 3: Risk of bias summary of randomized controlled trials pertaining the use of pericapsular nerve group block in hip surgeries.
After its first description as part of a multimodal analgesic regimen in five patients admitted with hip fracture diagnosis60, PENG block has been studied for analgesia in hip fracture patients11, postoperative analgesia in hip arthroscopy39 and postoperative analgesia and motor blockade in THA12-14,38,41.
Hip Fracture
In the single retained trial studying PENG block in the context of patients with hip fracture, Lin et al.11 compared PENG block to femoral nerve block (FNB) in patients undergoing surgery, including intra- and extracapsular fractures. Differently from the first reported experience of Girón-Arango et al., in this study the allocated block was performed 15-45 minutes before surgery and both techniques received 20 mL of 0.75% ropivacaine. Surgical technique and type of anesthesia were performed at the discretion of the treating physicians and the primary outcome was the postoperative pain measured in the post-anesthetic care unit (PACU) 4 hours after surgery. As a result, significant differences were found in terms of pain in the PACU but not on the postoperative day (POD) 1. Although the quadriceps strength was significantly more preserved with PENG block, interestingly 33% of patients in this group had a reduced or absent quadriceps strength in PACU and 7% on POD 1. Regarding postoperative complications, there were no differences. Regretfully, the level of pain assessment immediately after the block and a sub-analysis between intra- and extracapsular fractures, or types of surgeries, were not performed, thus, limiting the possible conclusions of this study.
Hip Arthroscopy
Just one trial investigating the benefits of PENG block in arthroscopic hip surgery has been published and has met the criteria for retention and further analysis in this review39. Amato et al. hypothesized that a PENG block with 20 mL of 0.5% ropivacaine would provide superior analgesia compared with a sham block. Seventy patients undergoing hip arthroscopy under standardized general anesthesia, multimodal analgesia, and local infiltration anesthesia of port sites with 30 mL of 0.25% bupivacaine were randomized and received the block prior to the intervention. The primary outcome was the worst reported pain score within 30 minutes after emergence from general anesthesia. Secondary outcomes included pain at 24hrs, opioid consumption, patient satisfaction, and opioid-related side effects. No differences were found for primary or secondary outcomes. Remarkably, the reported worst pain was moderate to severe in both groups, averaging numeric rating scores of 6.0 (2.6), 7.4(1.5) and 6.5 (1.7) at 30 minutes, 24hrs and 48hrs, respectively, in the PENG group. The postoperative motor blockade was not included among the evaluated outcomes.
Primary Total Hip Arthroplasty
Among the nine published trials researching PENG block for THA, five trials were selected for final analysis12-14,38,41.
Pascarella et al.38 compared a preoperative PENG block with 20 mL of 0.375% ropivacaine to no block in patients receiving spinal anesthesia and postoperative wound infiltration by surgeons. Additionally, the patients received multimodal systemic analgesia, including intraoperative dexamethasone 0.1mg/Kg. The primary outcome, postoperative pain, was significantly lower in the PENG block group. Among secondary outcomes, the opioid consumption and functional outcomes were better with PENG block, but there were no differences in terms of length of stay (LOS). Motor blockade was just assessed 24 hrs after surgery and focused on hip flexion and not on leg extension. In a similar trial41, Zheng et al. randomized 71 subjects to a preoperative PENG block with 20 mL of 0.5% ropivacaine or a sham block with 20 mL of normal saline solution. Both groups received general anesthesia and a postoperative intraarticular injection of 20 mL of 0.5% ropivacaine. The authors looked for a 33% decrease in the highest postoperative pain score at PACU and confirmed it. However, no significant differences were found either for pain scores later or for postoperative opioid consumption up to 48 hrs after surgery. Different from Pascarella's study38, Zheng assessed the sensory block 30 minutes after its performance and motor and sensory blockade in PACU and at 6hrs, 24 hrs and 48 hrs after surgery. Surprisingly, sensory block was present, without differences, in both groups during the PACU stay. Regarding the quadriceps strength, there were no significant between-group differences on either the operated side or the non-operated side during the study period.
Two trials compared the PENG block with a suprainguinal fascia iliac block (SIFIB)12,13. First, Choi et al.13 hypothesized that the PENG block with 20 mL of adrenalized 0.2% ropivacaine would provide better analgesia and less quadriceps weakness than a SIFIB with 30 mL of the same solution. The blocks were performed preoperatively after general anesthesia induction in 58 patients. The primary outcomes were pain scores at rest and during 45º passive hip flexion up to 48 h following surgery. Pain scores just differed at rest at 6 and 24hrs, but not in other timeframes or during movement. The postoperative opioid consumption was similar in both blocks. Hip flexion and knee extension were assessed preoperatively and 6 hrs, 24 hrs and 48 hrs after surgery. Surprisingly, compared with preoperative values, the quadriceps strength was similarly decreased in the two groups. Differing from Choi et al.'s protocol, Aliste et al.12 randomized 40 subjects undergoing THA under spinal anesthesia and sedation to receive a postoperative PENG block with 20 mL of adrenalized 0.5% bupivacaine or a SIFIB with 40 mL of adrenalized 0.25% bupivacaine. The primary outcome of this trial was the incidence of quadriceps motor block at 6 hrs after surgery. As a result, motor blockade was significantly more frequent in the SIFIB patients at 3 hrs and 6 hrs, without differences in pain scores, opioid consumption, ability to perform physiotherapy or LOS. Unexpectedly, the incidence of quadriceps weakness in the PENG group reached 45% and 25% at 3 hrs and 6 hrs.
In an Aliste et al.'s follow-up trial14, Bravo et al., in 60 patients undergoing THA under spinal anesthesia and sedation, compared PENG block to a periarticular local anesthetic infiltration (PAI) with 60 mL of adrenalized 0.25% bupivacaine. This time, the primary outcome was the incidence of quadriceps blockade at 3 hrs after surgery, hypothesizing that PAI would decrease its occurrence. However, unanticipatedly, and not differing from the PENG block group, the incidence of motor block with the selected PAI technique reached 33% and 13% at 3 hrs and 6 hrs, respectively. Additionally, the PAI group had less postoperative static pain in all evaluated intervals and less active pain at 3 hrs and 6 hrs after surgery. Furthermore, no intergroup differences were found in terms of sensory block or motor block at other time intervals; time to first opioid request; cumulative breakthrough morphine consumption; opioid-related side effects; ability to perform physiotherapy; and LOS.
In summary, for THA, no trial has compared the PENG block to a no regional technique group. In Pascarella´s38 a wound infiltration was performed at the end of surgery in both groups in the context of spinal anesthesia. The preoperative PENG block determined better pain management with less opioid requirement and improved range of motion and time to first walk. Zheng et al. proved that a preoperative PENG block in addition to an intraarticular injection of LA in patients under general anesthesia just determined differences in pain scores at PACU but not later41. In general, in both trials, the reported static and dynamic pain level was mild for PENG block patients. When directly compared to alternative techniques, the PENG block offers similar analgesia to SIFIB12,13. However, in the context of spinal anesthesia, in Aliste et al.'s trial12, the reported pain scores were milder than in Choi et al.'s13, where patients received general anesthesia. Both studies used standardized multimodal systemic analgesia in both study arms. More recently, when Bravo et al. compared the PENG block to PAI, PAI showed a better analgesic performance. Although in both groups, static and dynamic pain was mild, and there were no differences in other relevant outcomes14.
In the context of hip fracture surgery, Lin et al. showed a better analgesic performance of PENG block than FNB just in the PACU but did not do so later, with a similar opioid consumption during hospital stay11.
In arthroscopic hip surgery, Amato et al. demonstrated that PENG block does not improve immediate postoperative pain, at least when performed preoperatively, in patients under general anesthesia39.
Finally, regarding the timing of the block in the hip perioperative setting, in the seven RCTs retained in this review, the PENG block was performed prior to surgery, except for the group of Aliste and Bravo, who performed it postoperatively12,14. Independently of the timing and apart from the trial of Amato et al.39, the PENG block determined adequate postoperative analgesia but also decreased quadriceps strength when assessed. Direct comparisons between pre and postoperative PENG blocks have not been conducted and may help to elucidate the optimal timing for the block, both for analgesia and motor-sparing effects.
Complications of PENG Blocks
Since 2018, no study has reported specific complications related to PENG block. However, as with any block, potential injuries to surrounding structures are possible when the necessary conditions to execute a regional technique are not available.
Although not a complication, postoperative quadriceps paresis and paralysis have been reported in several publications and the possible mechanisms for it have been described previously in this article. In general, it has represented a transitory condition that has not delayed physiotherapy and hospital discharge. Additionally, the PAI, which might have represented a better motor-sparing alternative to the PENG block, has also been related to motor blockade requiring further research in order to find the best technique for it.
In summary, the literature accumulated over the last four years suggests that PENG blocks are not associated with severe complications.
Alternative Anterior Pericapsular Blocks
So far, only the iliopsoas plane block (IPB) has emerged as a comparator to the PENG block. Nielsen et al. have proposed a technical alternative to achieve an improved spread of LA into the iliopsoas space with the aim of reducing the incidence of quadriceps motor block61. A cadaveric study from the same group postulates that all sensory hip branches of the FN must pass through the anatomical plane between the IPM and the iliofemoral ligament, the so-called iliopsoas plane (IPP)22. There is a ligamentous IPP that extends inferolaterally from the acetabular rim and a muscular IPP, a complex formed by the ImM and IM with their lateral and medial fibers, which is a potential space between the capsular ligaments of the hip and the iliopsoas complex. As the ImM grows caudally, the IPP becomes an L-shaped fascial plane formed vertically by the muscular IPP and horizontally by the ligamentous IPP. In the IPB, the needle tip position lies at the junction of the muscular and ligamentous IPP. Nielsen et al. suggest that an injection of LA in this plane will provide regional analgesia of the articular sensory branches from the femoral nerve to the hip joint without spreading to any motor branches22. Thus, keeping the needle tip more laterally away from the undersurface of the IPT may help reduce the risk of incidental iliopectineal bursa injection and its resultant bursal rupture/puncture, which may continue anteromedially to flood the femoral nerve causing undesired quadriceps weakness19. Currently, there are no trials directly comparing the PENG block and the IPB.
Future Research
The PENG block has become an attractive analgesic alternative for different types of hip surgery. Despite its popularity, well-designed trials are still needed to elucidate some technical aspects in order to identify clear indications and control excessive expectations.
From an anatomical standpoint, clinical research inquiring into the articular branches will always be limited by the possibility of assessing the resulting block. Hence, a combination of cadaveric, imaging, and clinical studies (i.e., presence or absence of cutaneous or motor block) will be necessary. Thus, defining the optimal dosing volume seems to be the paramount element to revise. However, since different patterns of spread have been observed when tissue is distorted, logic dictates that settings such as underlying pathology (i.e., fracture, arthrosis, dysplasia) and surgical timing (pre, intra or post-surgery) should be added to the equation.
When analyzing the technical aspects of the block, besides some variations in the selection of the LA, its concentration, and the addition of adrenaline in the injectate, all the trials analyzed in this review maintained the arbitrary 20 mL volume selected by Giron-Arango et al. on their first report3. Up to now, no adequately designed and registered study has compared different technical aspects like injection sites, number of injections, LAs, concentration, volume, adjuvants, or continuous techniques. After the reported incidence of motor block with the original technique, it looks plausible that researching variations might permit finding an ideal approach to the pericapsular nerves group when early aggressive rehabilitation requiring optimal quadriceps function is needed. Furthermore, after the study of Bravo et al.14 it is possible that future research will turn into improving the analgesic qualities of the PENG block or, alternatively, look to decrease the motor blockade described with PAI. Certainly, both techniques still have a margin for improvement.
In terms of indications, THA seems to be the clearest since the PENG block determined adequate analgesia and low opioid consumption in all the trials analyzed in this review. Besides the results of Bravo et al.14, the better analgesic performance of PAI still needs to be corroborated by properly empowered trials. However, independently of what happens with PAI, the PENG block will probably keep having a role in centers where surgeons do not perform local anesthetic infiltration consistently and with good results.
Alternatively, in hip fracture cases, it is necessary to decrease the heterogeneity of protocols in order to validate the indication. For instance, when studying the analgesic role in subjects waiting for surgery, a distinction between intra and extracapsular fractures is needed. Similarly, different types of surgeries need to be studied separately. After all, the benefits may change from percutaneous fixations to arthroplasties. In contrast, secondary to the periarticular infiltrative characteristic of arthroscopic procedures, perhaps future studies need to reconsider the indication, timing, and ideal block technique (if any) for this surgery.
Agreeing with previous efforts to mitigate the reporting bias related to popular technical innovations40, we followed a similar approach to provide readers with a conservative reading of available RCTs. Thus, we have also purposefully excluded all trials that did not implement blinded assessment, sample size justification or trial registration. Also, we systematically excluded all RCTs displaying discrepancies between registered and reported protocols. Thus, maybe erring on the side of precaution, our analysis permits recommending the use of PENG blocks in hip replacement surgery when the possibility of quadriceps weakness in the immediate postoperative hours does not represent a delay with the plan of rehabilitation.
References
- Anger M, Valovska T, Beloeil H, et al. PROSPECT guideline for total hip arthroplasty: a systematic review and procedureâspecific postoperative pain management recommendations. Anaesthesia. 2021; 76: 1082-97. https://doi.org/10.1111/anae.15498
- Ræder J. SP53 PROSPECT guideline for pain management after hip fracture repair surgery: a systematic review and procedure-specific postoperative pain management recommendations. Invit Speak. 2022: A62: 2-A62. https://doi.org/10.1136/rapm-2022-esra.59
- Layera S, Saadawi M, Tran DQ, et al. Motor-Sparing Peripheral Nerve Blocks for Shoulder, Knee, and Hip Surgery. Adv Anesthesia. 2020; 38: 189-207. https://doi.org/10.1016/j.aan.2020.08.003
- Tran DQ, Salinas FV, Benzon HT, et al. Lower extremity regional anesthesia: essentials of our current understanding. Regional Anesthesia Pain Medicine. 2019; 44: 143. https://doi.org/10.1136/rapm-2018-000019
- Girón-Arango L, Peng PWH, Chin KJ, et al. Pericapsular Nerve Group (PENG) Block for Hip Fracture. Region Anesth Pain M. 2018; 43: 859-63. https://doi.org/10.1097/aap.0000000000000847
- Tran J, Agur A, Peng P. Is pericapsular nerve group (PENG) block a true pericapsular block? Regional Anesthesia Pain Medicine. 2019; 44: 257. https://doi.org/10.1136/rapm-2018-100278
- Aydin ME, Borulu F, Ates I, et al. A Novel Indication of Pericapsular Nerve Group (PENG) Block: Surgical Anesthesia for Vein Ligation and Stripping. J Cardiothor Vasc An. 2020; 34: 843-5. https://doi.org/10.1053/j.jvca.2019.08.006
- Ahiskalioglu A, Aydin ME, Ozkaya F, et al. A novel indication of Pericapsular Nerve Group (PENG) block: Prevention of adductor muscle spasm. J Clin Anesth. 2020; 60: 51-2. https://doi.org/10.1016/j.jclinane.2019.08.034
- Ahiskalioglu A, Aydin ME, Celik M, et al. Can high volume pericapsular nerve group (PENG) block act as a lumbar plexus block? J Clin Anesth. 2020; 61: 109650. https://doi.org/10.1016/j.jclinane.2019.109650
- Ahiskalioglu A, Aydin ME, Ahiskalioglu EO, et al. Pericapsular nerve group (PENG) block for surgical anesthesia of medial thigh. J Clin Anesth. 2020; 59: 42-3. https://doi.org/10.1016/j.jclinane.2019.06.021
- Lin D-Y, Morrison C, Brown B, et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: a single-center double-blinded randomized comparative trial. Regional Anesthesia Pain Medicine. 2021; 46: 398-403. https://doi.org/10.1136/rapm-2020-102315
- Aliste J, Layera S, Bravo D, et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Regional Anesthesia Pain Medicine. 2021; 46: 874-8. https://doi.org/10.1136/rapm-2021-102997
- Choi YS, Park KK, Lee B, et al. Pericapsular Nerve Group (PENG) Block versus Supra-Inguinal Fascia Iliaca Compartment Block for Total Hip Arthroplasty: A Randomized Clinical Trial. J Personalized Medicine. 2022; 12: 408. https://doi.org/10.3390/jpm12030408
- Bravo D, Aliste J, Layera S, et al. Randomized clinical trial comparing pericapsular nerve group (PENG) block and periarticular local anesthetic infiltration for total hip arthroplasty. Regional Anesthesia Pain Medicine. 2023. https://doi.org/10.1136/rapm-2023-104332
- Gardner E. The innervation of the hip joint. Anat Rec. 1948; 101: 353-71. https://doi.org/10.1002/ar.1091010309
- Short AJ, Barnett JJG, Gofeld M, et al. Anatomic Study of Innervation of the Anterior Hip Capsule: Implication for Image-Guided Intervention. Region Anesth Pain M. 2018; 43: 186-92. https://doi.org/10.1097/aap.0000000000000701
- Delmas A, Rouvière H. Anatomía Humana descriptiva, topográfica y funcional n.d.
- Nielsen TD, Moriggl B, Barckman J, et al. Cutaneous anaesthesia of hip surgery incisions with iliohypogastric and subcostal nerve blockade: A randomised trial. Acta Anaesth Scand. 2019; 63: 101-10. https://doi.org/10.1111/aas.13221
- Yeoh S-R, Chou Y, Chan S-M, et al. Pericapsular Nerve Group Block and Iliopsoas Plane Block: A Scoping Review of Quadriceps Weakness after Two Proclaimed Motor-Sparing Hip Blocks. Healthc. 2022; 10: 1565. https://doi.org/10.3390/healthcare10081565
- Barker JP, Yang Y, Matz J, et al. The Iliopectineal Fascia: A Cadaveric Anatomical Study. J Orthop Trauma. 2021; 35: 333-8. https://doi.org/10.1097/bot.0000000000001995
- Gerhardt M, Johnson K, Atkinson R, et al. Characterisation and Classification of the Neural Anatomy in the Human Hip Joint. HIP International. 2011; 22: 75-81. https://doi.org/10.5301/HIP.2012.9042
- Nielsen ND, Greher M, Moriggl B, et al. Spread of injectate around hip articular sensory branches of the femoral nerve in cadavers. Acta Anaesth Scand. 2018; 62: 1001-6. https://doi.org/10.1111/aas.13122
- Kitcharanant N, Leurcharusmee P, Wangtapun P, et al. Surgeon-performed pericapsular nerve group (PENG) block for total hip arthroplasty using the direct anterior approach: a cadaveric study. Regional Anesthesia Pain Medicine. 2022; 47: 359-63. https://doi.org/10.1136/rapm-2022-103482.
- Aksu C, Cesur S, KuÅ A. Pericapsular nerve group (PENG) block for postoperative analgesia after open reduction of pediatric congenital dysplasia of the hip. J Clin Anesth. 2020; 61: 109675. https://doi.org/10.1016/j.jclinane.2019.109675
- Yu HC, Moser JJ, Chu AY, et al. Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Regional Anesthesia Pain Medicine. 2019; 44: 611-3. https://doi.org/10.1136/rapm-2018-100354
- Girón-Arango L, Roqués V, Peng P. Reply to Dr Roy et al: Total postoperative analgesia for hip surgeries: PENG block with LFCN block. Regional Anesthesia Pain Medicine. 2019; 44: 684.2-685. https://doi.org/10.1136/rapm-2019-100505
- Black ND, Chin KJ. Pericapsular nerve group (PENG) block: Comments and practical considerations. J Clin Anesth. 2019; 56: 143-4. https://doi.org/10.1016/j.jclinane.2019.02.010
- Jadon A, Sinha N, Chakraborty S, et al. Pericapsular nerve group (PENG) block: A feasibility study of landmark based technique. Indian J Anaesth. 2020; 64: 710-3. https://doi.org/10.4103/ija.ija_388_20
- Yavuz F, Yasar E, Taskaynatan M, et al. Nerve block of articular branches of the obturator and femoral nerves for the treatment of hip joint pain. Journal of Back and Musculoskeletal Rehabilitation. 2013; 26: 79-83. https://doi.org/10.3233/bmr-2012-00353
- Arango LG, Peng P. Reply to Dr Yu et al: Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Regional Anesthesia Pain Medicine. 2019; 44: 613-4. https://doi.org/10.1136/rapm-2018-100263
- Girón-Arango L, Tran J, Peng PW. Reply to Aydin et al: A Novel Indication of Pericapsular Nerve Group Block: Surgical Anesthesia for Vein Ligation and Stripping. J Cardiothor Vasc An. 2020; 34: 845-6. https://doi.org/10.1053/j.jvca.2019.10.027
- Fusco P, Carlo SD, Paladini G, et al. Could the combination of PENG block and LIA be a useful analgesic strategy in the treatment of postoperative pain for hip replacement surgery? Regional Anesthesia Pain Medicine. 2019; 44: 531-531. https://doi.org/10.1136/rapm-2018-100277
- Peng PWH, Perlas A, Chin KJ. Reply to Dr Nielsen: Pericapsular Nerve Group (PENG) block for hip fracture. Regional Anesthesia Pain Medicine. 2019; 44: 415. https://doi.org/10.1136/rapm-2018-100234
- Endersby RVW, Moser JJ, Ho ECY, et al. Motor blockade after iliopsoas plane (IPB) and pericapsular nerve group (PENG) blocks: A little may go a long way. Acta Anaesth Scand. 2021; 65: 135-6. https://doi.org/10.1111/aas.13707
- Altinpulluk EY, Galluccio F, Salazar C, et al. Peng block in prosthetic hip replacement: A cadaveric radiological evaluation. J Clin Anesth. 2020; 65: 109888. https://doi.org/10.1016/j.jclinane.2020.109888
- Ciftci B, Ahiskalioglu A, Altintas HM, et al. A possible mechanism of motor blockade of high volume pericapsular nerve group (PENG) block: A cadaveric study. J Clin Anesth. 2021; 74: 110407. https://doi.org/10.1016/j.jclinane.2021.110407
- Kim JY, Kim J, Kim D-H, et al. Anatomical and Radiological Assessments of Injectate Spread Stratified by the Volume of the Pericapsular Nerve Group Block. Anesthesia Analgesia. 2023; 136: 597-604. https://doi.org/10.1213/ane.0000000000006364
- Pascarella G, Costa F, Buono RD, et al. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: a randomised, observer‑masked, controlled trial. 2021; 76: 1492-8. https://doi.org/10.1111/anae.15536
- Amato PE, Coleman JR, Dobrzanski TP, et al. Pericapsular nerve group (PENG) block for hip arthroscopy: a randomized, double-blinded, placebo-controlled trial. Regional Anesthesia Pain Medicine. 2022; 47: 728-32. https://doi.org/10.1136/rapm-2022-103907
- Tran DQ, Sites BD. Discrepancy between registered and reported trial protocols: don’t ask, don’t tell or zero tolerance? Regional Anesthesia Pain Medicine. 2020; 45: 253. https://doi.org/10.1136/rapm-2019-101128
- Zheng J, Pan D, Zheng B, et al. Preoperative pericapsular nerve group (PENG) block for total hip arthroplasty: a randomized, placebo-controlled trial. Regional Anesthesia Pain Medicine. 2022; 47: 155-60. https://doi.org/10.1136/rapm-2021-103228
- Güllüpınar B, saÄlam caner, Ünlüer EE, et al. Effectiveness of Pericapsular Nerve Group Block with Ultrasonography in Patients Diagnosed with Hip Fracture in the Emergency Department. Turkish J Trauma Emerg Surg. 2022. https://doi.org/10.14744/tjtes.2022.67817
- Hua H, Xu Y, Jiang M, et al. Evaluation of Pericapsular Nerve Group (PENG) Block for Analgesic Effect in Elderly Patients with Femoral Neck Fracture Undergoing Hip Arthroplasty. J Healthc Eng. 2022; 2022: 7452716. https://doi.org/10.1155/2022/7452716
- Reddy MD, P SSM, Sahithi B, et al. Comparison of Pericapsular Nerve Group Block (PENG) Versus Fascia Iliaca Compartment Block (FICB) as Postoperative Pain Management in Hip Fracture Surgeries. Journal of Cardiovascular Disease Research. 2022.
- Jadon A, Mohsin K, Sahoo RK, et al. Comparison of supra-inguinal fascia iliaca versus pericapsular nerve block for ease of positioning during spinal anaesthesia: A randomised double-blinded trial. Indian J Anaesth. 2021; 65: 572-8. https://doi.org/10.4103/ija.ija_417_21
- Mosaffa F, Taheri M, Rasi AM, et al. Comparison of pericapsular nerve group (PENG) block with fascia iliaca compartment block (FICB) for pain control in hip fractures: A double-blind prospective randomized controlled clinical trial. Orthop Traumatology Surg Res. 2022; 108: 103135. https://doi.org/10.1016/j.otsr.2021.103135
- Lin D-Y, Brown B, Morrison C, et al. Pericapsular nerve group block results in a longer analgesic effect and shorter time to discharge than femoral nerve block in patients after hip fracture surgery: a single-center double-blinded randomized trial. J Int Med Res. 2022; 50: 03000605221085073. https://doi.org/10.1177/03000605221085073
- Natrajan P, Bhat RR, Remadevi R, et al. Comparative Study to Evaluate the Effect of Ultrasound-Guided Pericapsular Nerve Group Block Versus Fascia Iliaca Compartment Block on the Postoperative Analgesic Effect in Patients Undergoing Surgeries for Hip Fracture under Spinal Anesthesia. Anesthesia Essays Res. 2021; 15: 285-9. https://doi.org/10.4103/aer.aer_122_21
- Senthil KS, Kumar P, Ramakrishnan L. Comparison of Pericapsular Nerve Group Block versus Fascia Iliaca Compartment Block as Postoperative Pain Management in Hip Fracture Surgeries. Anesthesia Essays Res. 2021; 15: 352-6. https://doi.org/10.4103/aer.aer_119_21
- Lin D-Y, Brown B, Morrison C, et al. The Pericapsular Nerve Group (PENG) block combined with Local Infiltration Analgesia (LIA) compared to placebo and LIA in hip arthroplasty surgery: a multi-center double-blinded randomized-controlled trial. Bmc Anesthesiol. 2022; 22: 252. https://doi.org/10.1186/s12871-022-01787-2
- Kong M, Tang Y, Tong F, et al. The analgesic efficacy of pericapsular nerve group block in patients with intertrochanteric femur fracture: A randomized controlled trial. Plos One. 2022; 17: e0275793. https://doi.org/10.1371/journal.pone.0275793
- Hu J, Wang Q, Hu J, et al. Efficacy of ultrasound-guided pericapsular nerve group (PENG) block combined with local infiltration analgesia on postoperative pain after total hip arthroplasty: a prospective, double-blind, randomized controlled trial. J Arthroplast. 2022. https://doi.org/10.1016/j.arth.2022.12.023
- Iglesias SL, Nieto I, López P, et al. Bloqueo De Nervios Pericapsulares (Peng) Es Una Alternativa Efectiva Y Segura Para El Manejo Del Dolor Postoperatorio Luego De Una Artroplastia Total De Cadera Primaria: Ensayo Clínico Aleatorizado. Revista Española De Cirugía Ortopédica Y Traumatología. 2022. https://doi.org/10.1016/j.recot.2022.12.004
- Chung CJ, Eom DW, Lee TY, et al. Reduced Opioid Consumption with Pericapsular Nerve Group Block for Hip Surgery: A Randomized, Double-Blind, Placebo-Controlled Trial. Pain Res Management. 2022; 2022: 6022380. https://doi.org/10.1155/2022/6022380
- Kalashetty MB, Channappagoudar R, Alwandikar V, et al. Comparison of Pericapsular Nerve Group Block with Fascia Iliaca Compartment Block in Adult Patients Undergoing Hip Surgeries: A Double-Blinded Randomized Control Study. Anesthesia Essays Res. 2022; 16: 397-401. https://doi.org/10.4103/aer.aer_123_22
- Balasubramaniam A, NAGGAIH SK, Tarigonda S, et al. Ultrasound-Guided Pericapsular Nerve Group Block for Hip Surgery: A Randomized Controlled Trial Study Comparing Ropivacaine and Ropivacaine With Dexamethasone. Cureus J Medical Sci. 2023; 15: e34261. https://doi.org/10.7759/cureus.34261
- Zheng L, Jo Y, Hwang J, et al. Comparison of the analgesic efficacy of periarticular infiltration and pericapsular nerve group block for total hip arthroplasty: a randomized, non-inferiority study. Ann Palliat Medicine. 2021. https://doi.org/10.21037/apm-21-2785
- Alrefaey AK, Abouelela MA. Pericapsular nerve group block for analgesia of positioning pain during spinal anesthesia in hip fracture patients, a randomized controlled study. Egypt J Anaesth. 2020; 36: 234-9. https://doi.org/10.1080/11101849.2020.1828017
- Alshawadfy A, Elewa AM, Mewafy MA, et al. Comparison between pericapsular nerve group block and morphine infusion in reducing pain of proximal femur fracture in the emergency department: A randomized controlled study. Egypt J Anaesth. 2023; 39: 26-31. https://doi.org/10.1080/11101849.2023.2165888
- ElHalim MAGA, Saleh AA, Alqassas MH. PENG (Pericapsular Nerve Group) block versus intravenous fentanyl as an analgesic technique in cardiac patients for positioning ofhip fracture: Prospective, Randomized study. Journal of Cardiovascular Disease Research. 2021.
- Nielsen ND, Madsen MN, Østergaard HK, et al. An iliopsoas plane block does not cause motor blockade—A blinded randomized volunteer trial. Acta Anaesth Scand. 2020; 64: 368-77. https://doi.org/10.1111/aas.13498
Appendix 1
Discarded randomized trials and reason for non-inclusion
|
Trial |
Comparison |
Main reason for no inclusion |
|
Gullupinar et al. 202242 |
PENGB vs Control |
No prospective trial registration
|
|
Hua et al. 202143 |
PENGB vs SIFIB |
No prospective trial registration |
|
Reddy et al. 202244 |
PENGB vs SIFIB |
No prospective trial registration |
|
Jadon et al. 202145 |
PENGB vs SIFIB |
No prospective trial registration (no code offered) |
|
Mossafa et al. 202246 |
PENGB vs FIB |
No prospective trial registration, Discrepancy between registered (36) and reported (52) sample sizes |
|
Lin et al. 202247 |
PENGB vs FNB |
Not a trial but sub-analysis of a previous one |
|
Natrajan et al. 202248 |
PENGB vs FIB |
No prospective trial registration |
|
Senthil et al. 202249 |
PENGB vs SIFIB |
No prospective trial registration |
|
Lin et al. 202250 |
PENG+LIA vs LIA |
Discrepancy between registered (36) and reported (60) sample sizes |
|
Kong et al. 202251 |
PENGB vs FIB |
Discrepancy between registered (200) and reported |
|
Hu et al. 202252 |
PENG+LIA vs LIA |
No prospective trial registration |
|
Iglesias et al. 202253 |
PENG vs PNB vs PAI |
No prospective trial registration |
|
Chung et al. 202254 |
PENG vs Control |
No prospective trial registration |
|
Kallashetty et al. 202255 |
PENGB vs FIB |
No prospective trial registration (recruitment started in January 2020 and register occurred in July 2020) |
|
Balasubramaniam et al. |
PENGB vs PENGB + dexamethasone |
No prospective trial registration |
|
Zheng et al. 202257 |
PENG vs PAI |
No prospective trial registration |
|
Alrefaey et al. 202058 |
PENGB vs Control |
Discrepancy between registered (50) and reported (60) sample sizes, primary (morphine vs pain in positioning) and secondary outcomes |
|
Alshawadfy et al. 202359 |
PENGB vs Control |
Discrepancy between registered (60) and reported (36) sample sizes |
|
ElHalim et al. 202160 |
PENGB vs Fentanil |
No prospective trial registration
|
PENGB= pericapsular nerve group block; LIA= local infiltration anesthesia; PAI=periarticular local anesthetic infiltration; SIFIB= suprainguinal fascia iliaca block; FIB= fascia iliaca block; FNB= femoral nerve block.
