Navigating Challenges During Airway Management and Anesthetic Considerations in a Patient with a Supraglottic Mass: Integrating Anesthesiologists and Otolaryngologist Expertise
Najah Arafat Albayedh1*, Muzan Abdelbagi1, Yasser Samir Elmehellawy2, Ragai Abdelbasset Gemi3, Omar Majed Abdul Baki2
1Department of Anesthesia and Critical Care medicine, Al-Qassimi hospital, Emirates Health Services (EHS), Sharjah, United Arab Emirates
2Department of Anesthesia, Al-Qassimi hospital, Emirates Health Services (EHS), Sharjah, United Arab Emirates
3Department of Ear, Nose, and Throat (ENT), Al-Qassimi hospital, Emirates Health Services (EHS), Sharjah, United Arab Emirates. Professor of ENT, Cairo University, Cairo, Egypt
Abstract
Introduction: Managing patients undergoing head and neck surgeries necessitates meticulous evaluation, strategic planning, and collaborative efforts with surgical teams. This approach is crucial to mitigate perioperative complications and optimize patient safety.
Rationale: Expert navigation of the challenging airway in these patients, particularly in the perioperative period, is essential to significantly reduce the risks of morbidity and mortality associated with such complex conditions.
Patient Concerns and Diagnosis: The patient presented with a supraglottic mass extending into the epiglottis space, posing significant anesthetic challenges to airway management.
Outcomes: A surgical airway was established via tracheostomy. Postoperatively, the patient was monitored in the intensive care unit for further management and was subsequently discharged to commence chemoradiotherapy. The tracheostomy tube remained in place at the time of discharge.
Lessons: This case underscored our commitment to enhancing expertise in airway management for patients with oral cancer. Our experience contributes valuable insights to the evolving field of airway management in complex head and neck surgeries.
Introduction: Airway Management Challenges in Non-Hodgkin’s Lymphoma of the Oral Cavity
Non-Hodgkin’s lymphoma is not a common encounter and representing approximately only one percent of oral cavity cancers1, presents unique challenges in clinical practice, particularly in airway management. The rarity of this malignancy results in a limited number of case reports in the literature, especially concerning difficulties encountered in airway management. Given its location in the head and neck region and the shared responsibility of management with otolaryngologists, comprehensive pre-evaluation is essential for adequately preparing at-risk patients for potential unforeseen complications. In the absence of established guidelines for difficult airway management in these patients, adopting a comprehensive strategy rather than relying on a singular plan is recommended2.
Case Presentation
A 78 kgs, 72-year old lady with history of hypertension, dyslipidemia and past surgical history of tonsillectomy was referred to the ear, nose and throat (ENT) clinic as a case of tongue cancer which was confirmed by computed tomography (CT) (Figure 1) of the head and neck at another hospital with a history of change in voice (hot potato speech) and noticed a progressive swelling on the right side of neck for one month. She has associated difficulty in swallowing with noisy breathing, but no stridor noted. All signs and symptoms imply the provisional diagnosis of supraglottic mass of the base of the tongue.
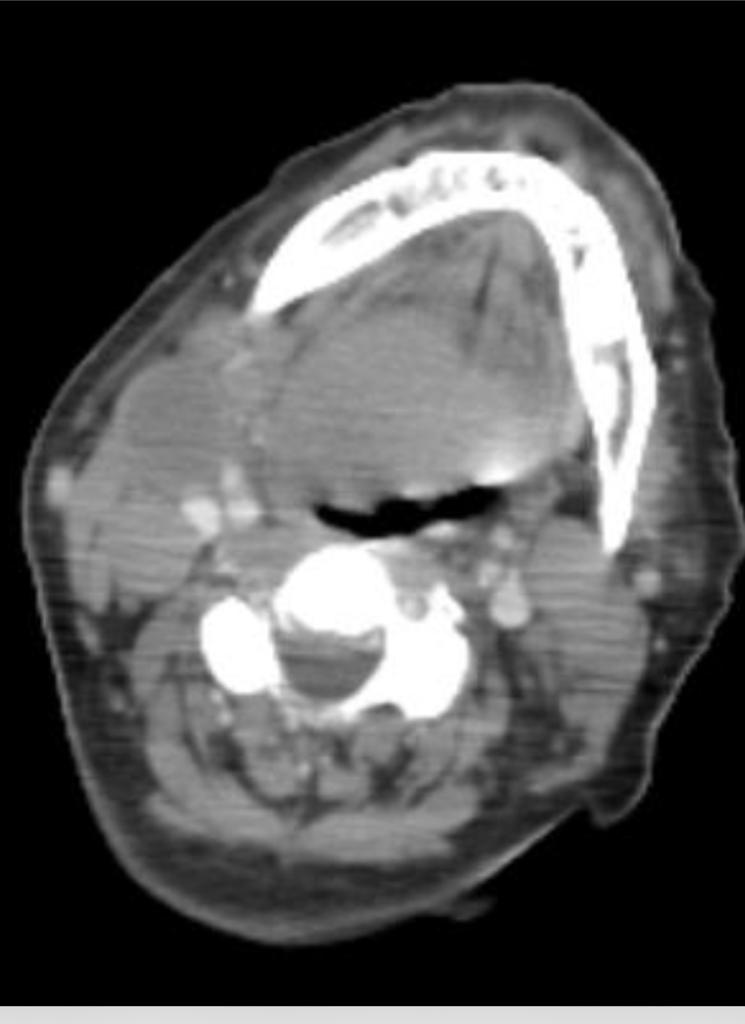
Figure 1: Pre-operative computerized tomography (CT) of the neck.
Physical examination of the neck showed bilateral level two and three cervical lymphadenopathy. Preoperative flexible laryngoscopy performed in the ENT clinic revealed an ulcero-proliferative lesion involving right base of tongue, extending to the right side vallecula and right side of epiglottis and aryepiglottic fold, obscuring the view of vocal cords.
Upon pre-Anesthesia evaluation of the patient in the clinic, the preferred anesthesia technique’s was general anesthesia, awake flexible fiberoptic intubation was excluded due to several factors regarding the patient's airway such as inability to visualize the glottis and grossly distorted anatomy in the nasendoscopy findings as well as the patient’s uncooperative manner.
The patient is categorized as an American Society of Anesthesiologists (ASA) classification of II with normal cervical spine range of motion and mobility, no obvious jaw deformities, Mallampati class III, adequate thyromental distance and mouth opening.
CT scan of the soft tissue of the neck revealed homogeneously enhancing mass lesions in the posterior third of the tongue predominantly on the right causing significant airway narrowing.
The patient was then posted for a laryngoscopy and biopsy of the hypopharyngeal mass.
The patient and her family were informed about the possibility of it being a non-benign tumor, and the need of performing a biopsy with the risk of difficult intubation and risk of failure of extubation hence surgical tracheostomy was discussed with postoperative intensive care admission and ventilation.
Due to anticipation of difficult airway as evidenced by the aforementioned findings clinically and radiologically, we prepared microlaryngeal tube (MLT) sizes 5 and 5.5 mm, Glideoscope video laryngoscope, bougie, supraglottic airway devices and tracheostomy set.
The patient was pre-oxygenated for three minutes then fentanyl 100 microgram, propofol 200 milligram and Rocuronium bromide 50 milligrams were administered. Sugammadex was readily available at our unit for reversal of Rocuronium. The Glideoscope video laryngoscope was used to explore the airway and stratify chances of successful intubation. It revealed a bulky mass obscuring the epiglottis and vocal cords (Figure 2). A bloody field urged us to utilize the bougie but failed to appropriately insert the tube and the patient started to desaturate which obliged us to bag-mask ventilation until saturation picked up (Figure 3). Upon the third try, the posterior segment of the vocal cords were better visualized. Bougie was directed towards it and the endotracheal tube was secured successfully (Figure 4), evidenced by bilateral chest rise, auscultation and end tidal carbon dioxide. A single dose of 8 mg dexamethasone has been administered.

Figure 2: First VL attempt revealing Cormack Lehane grade 3.
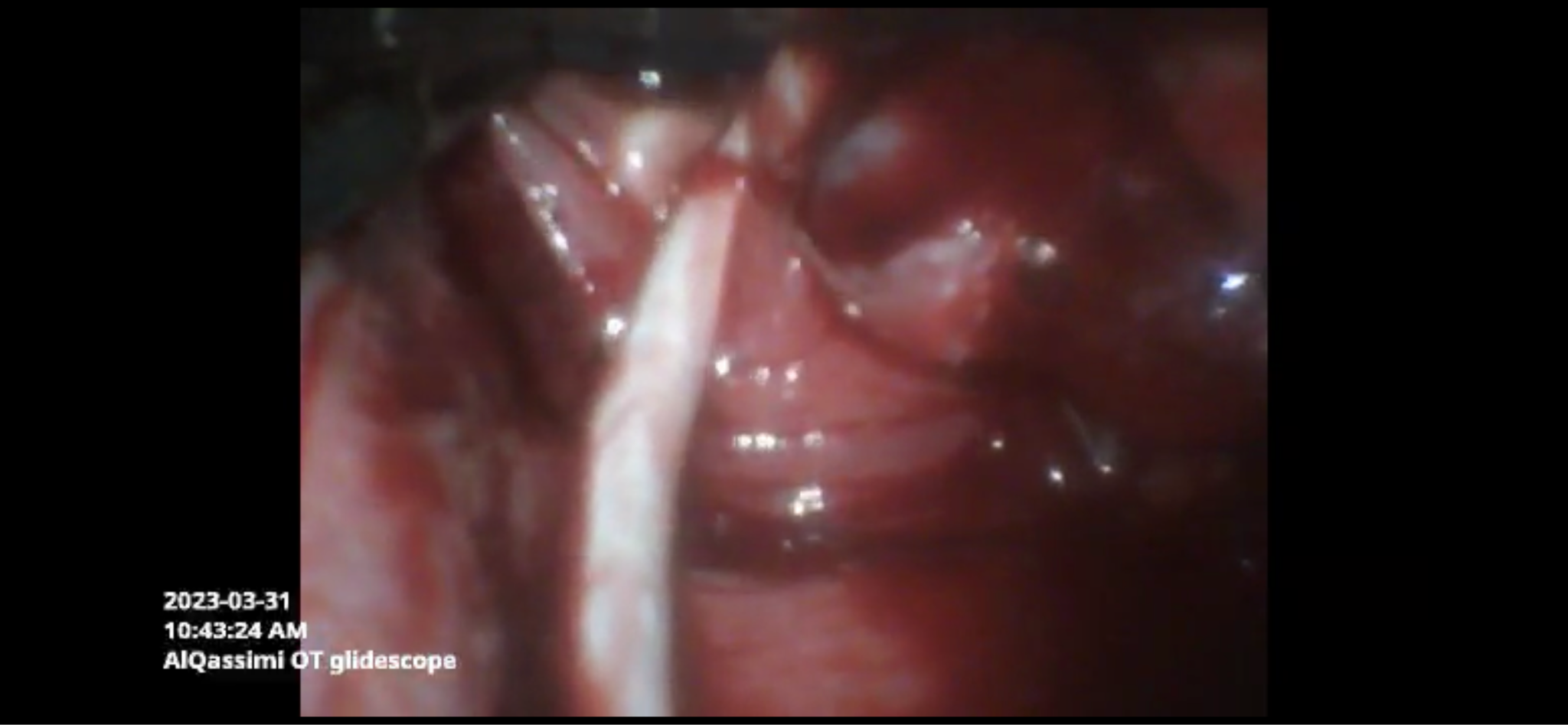
Figure 3: Second VL attempt showing a bloody field with insertion of bougie.

Figure 4: Upon third attempt, endotracheal intubation using bougie was successful.
A biopsy was taken from the mass and was sent for histopathology. Surgical tracheostomy under local anesthesia was performed as the mass was causing significant airway compromise, and the patient was transferred to the ICU for further management and observation. Histopathology examination showed atypical proliferation of lymphoid cells positive for B-cell suggestive of Non-Hodgkin’s lymphoma. A CT scan of the neck post chemotherapy is seen (Figure 5)

Figure 5: CT scan of the neck revealing reduction of size of the tumor post chemotherapy.
Discussion
Rare Manifestation of Lymphomas at the Tongue Base: Diagnostic and Surgical Challenges
Lymphomas occurring at the base of the tongue are extremely rare, as this site is not commonly associated with lymphoma development3. Early recognition of signs and symptoms indicative of airway obstruction in these cases is crucial. These symptoms include dyspnea (both at rest and during exertion), dysphagia, stridor, cough, and changes in voice quality. Notably, a muffled voice often suggests supraglottic disease, while glottic lesions typically produce a coarse, scratchy voice.
Perioperative Airway Complications in Head and Neck Surgeries
Head and neck surgical procedures are notably challenged by perioperative airway complications. About one-third of such cases experience these complications, with approximately 75% requiring emergency surgical airways (ESA)2. This is highlighted in a comprehensive Danish study, which observed a higher incidence of ESA among ENT patients—encompassing approximately 450,000 individuals with various pathologies, including head and neck conditions—compared to the general surgical population.
Anesthesia Induction and Airway Management Strategies
The induction of general anesthesia (GA) can worsen airway obstruction, making flexible fiberoptic scope intubation (FSI) a preferred method. FSI is advantageous for maintaining a patent airway and reducing the risk of aspiration, among other benefits4. However, FSI in head and neck surgeries often encounters high failure rates, attributed to factors like suspected bleeding, airway edema leading to obstruction, and difficulties in visualizing the glottis for scope passage5,6. In our case, awake fiberoptic intubation was considered unsuitable due to several patient-specific factors, including the inability to visualize the glottis, grossly distorted anatomy in nasendoscopy findings, and the patient’s non-cooperative demeanor.
Employment of Glidescope Video Laryngoscopy
As a result, we opted for Glidescope video laryngoscopy for endotracheal intubation, aiming to improve our first-pass success rate. This technique has been reported to effectively replace awake fiberoptic bronchoscopy-guided intubation and surgical airway procedures in certain cases7.
Cisatracurium in Micro Laryngeal Surgeries: Challenges and Alternatives
Recent studies have explored the use of Cisatracurium in micro laryngeal surgeries, noting its potential for residual neuromuscular blockade effects in the postoperative recovery unit, particularly in brief procedures. This phenomenon persists even with the use of Neostigmine to counteract these effects8,9,10. An alternative approach involving the combination of Rocuronium and Sugammadex has been identified as superior, offering improved intubation conditions and surgical outcomes. Fortunately, Sugammadex is readily available at our institution.
Difficult Tracheal Intubation in Head and Neck Surgeries
It is documented that up to 10% of head and neck surgeries encounter difficult tracheal intubations, defined as requiring three or more attempts at direct laryngoscopy. The friable nature of these cancers often leads to airway distortion, bleeding, fragmentation, rapid airway edema, and soiling during laryngoscopy. Compared to other elective surgeries, head and neck procedures exhibit a higher rate of complications both during emergence and post-extubation. These complications range from laryngospasm and postextubation airway edema to postoperative airway obstruction and the need for reintubation.
Surgical Tracheostomy: A Proactive Approach
Given the high risk of airway swelling and edema potentially compromising the airway, having a plan for surgical tracheostomy is crucial. Our patient consented to this approach initially. Performing tracheostomy under local anesthesia after induction is preferred to prevent airway trauma, particularly postoperatively, and to mitigate risks of obstruction and tumor seeding. This decision depends on several factors: the duration of the surgery, the likelihood of progressive swelling, and the risk of aspiration and field bleeding. In our case, tracheostomy offered several advantages, including a secure airway, improved bronchial hygiene, reduced dead space, and facilitated weaning from mechanical ventilation.
Navigating Difficult Airways in Laryngeal Tumors
Current algorithms for managing difficult airways do not offer specific guidance for cases involving laryngeal tumors. They provide a general framework for action in the event of an anticipated difficult airway. Therefore, it is essential to have a tailored plan, with readiness for procedures like cricothyrotomy or tracheostomy, given that approximately ninety percent of difficult airways are unforeseen11.
Corticosteroids and Chemotherapy in Lymphoid Malignancies
The role of corticosteroids in conjunction with chemotherapy for treating lymphoid malignancies is a critical consideration. Several meta-analyses have demonstrated the efficacy of corticosteroids in reducing the rates of reintubation and postextubation stridor12,13,14. These findings underscore the importance of corticosteroids in managing airway complications associated with lymphoid malignancies.
Tumor Lysis Syndrome: A Critical Oncological Concern
Tumor lysis syndrome (TLS) represents a significant oncological emergency, frequently reported following the initiation of cytotoxic chemotherapy. It is characterized by the rapid breakdown of large, aggressive tumors upon commencement of chemotherapy15. In our patient’s case, there has been no development of symptoms associated with TLS during the course of admission. Additionally, the administration of a single low dose of dexamethasone is unlikely to induce TLS, and no initiation of corticosteroid therapy has been reported from the referring hospital.
Case Reports of TLS during General Anesthesia
The literature includes a few case reports describing the onset of TLS during general anesthesia (GA). One such report involved a middle-aged woman presenting with TLS for cervical lymphadenopathy following the administration of 20 mg dexamethasone. The first documented instance of TLS occurring during GA was in 2001, involving a 12-year-old undergoing liver transplantation. This patient, who did not receive steroids during surgery, experienced TLS triggered by a biopsy of the lesion. Another case from early 2007 reported acute TLS at the end of a staging laparotomy for lymphoma. While the use of dexamethasone was not specified, the onset of hemodynamic instability was attributed to surgical stress and manipulation of the lesion. Notably, there has been a reported case of perioperative mortality due to acute TLS in a 3-year-old child, occurring 6 hours post elective adenotonsillectomy, with an undiagnosed acute lymphoblastic leukemia.
Conclusion
Non-Hodgkin's lymphoma hardly ever targets the tongue, but when it does, it can lead to serious problems like blocking the airway. In such cases, anesthesiologists and otolaryngologists should always think about the possibility of intubation failure. In conclusion, these findings underscore the significance of vigilant monitoring and preparedness in managing patients undergoing head and neck surgeries to minimize the risk of complications and ensure a safe and successful recovery process.
References
- Ahmed-Nusrath A. Anaesthesia for head and Neck Cancer surgery. BJA Education. 2017; 17(12): 383-389. doi:10.1093/bjaed/mkx028
- Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: Results of the fourth national audit project of the royal college of anaesthetists and the difficult airway society. part 1: Anaesthesia. British Journal of Anaesthesia. 2011; 106(5): 617-631. doi:10.1093/bja/aer058
- Chenthilnathan P, et al. Base of tongue as an unusual site for non-Hodgkin lymphoma. Bangladesh Journal of Medical Science. 2012; 11(3): 248-249. doi:10.3329/bjms.v11i3.11740
- Bryan YF, et al. Procedural challenges during intubation in patients with oropharyngeal masses: A prospective observational study. Anesthesia & amp; Analgesia. 2019; 128(6): 1256-1263. doi:10.1213/ane.0000000000004089
- Apfelbaum JL, et al. 2022 American Society of Anesthesiologists Practice Guidelines for management of the difficult airway. Anesthesiology. 2021; 136(1): 31-81. doi:10.1097/aln.0000000000004002
- Woodall N, Frerk C, Cook TM. Can we make airway management (even) safer? – lessons from national audit. Anaesthesia. 2011; 66(s2): 27-33. doi:10.1111/j.1365-2044.2011.06931.x
- Avidan A, et al. Difficult airway management practice changes after introduction of the Glidescope videolaryngoscope. European Journal of Anaesthesiology, Publish Ahead of Print. Available at: https://doi.org/10.1097/eja.0000000000001199
- Martinez-Ubieto J, Ortega-Lucea S, Pascual-Bellosta A, et al. Prospective study of residual neuromuscular block and postoperative respiratory complications in patients reversed with neostigmine versus sugammadex. Minerva anestesiologica. 2016; 82(7): 735-742.
- Butterly A, et al. Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. British Journal of Anaesthesia. 2010; 105(3): 304-309. Available at: https://doi.org/10.1093/bja/aeq157
- Murphy GS, Brull SJ. Residual neuromuscular block. Anesthesia & Analgesia. 2010; 111(1): 120-128. Available at: https://doi.org/10.1213/ane.0b013e3181da832d
- Wong P, et al. Head and Neck Surgery in a tertiary centre: Predictors of difficult airway and anaesthetic management. Proceedings of Singapore Healthcare. 2015; 25(1): 19-26. Available at: https://doi.org/10.1177/2010105815615995
- Kuriyama A, Umakoshi N, Sun R. Prophylactic corticosteroids for prevention of postextubation stridor and reintubation in adults: a systematic review and meta-analysis. Chest. 2017; 151: 1002-10. doi: 10.1016/j.chest.2017.02.017
- Fan T, Wang G, Mao B, et al. Prophylactic administration of parenteral steroids for preventing airway complications after extubation in adults: meta-analysis of randomised placebo controlled trials. BMJ. 2008; 337: a1841. doi: 10.1136/bmj.a1841
- McCaffrey J, Farrell C, Whiting P, et al. Corticosteroids to prevent extubation failure: a systematic review and meta-analysis. Intensive Care Med. 2009; 35: 977-86. doi: 10.1007/s00134-009-1473-9
- Kalamkerian G, Darwish B, Varterasian M. Tumour lysis syndrome, in small cell cancer and other solid tumors. American Journal of Medicine. 1997; 103: 363-7.
