Quadratus Lumborum Block for Post Caesarean Delivery Analgesia: A Review
Anudeep Jafra1, Jeetinder Kaur Makkar1*, Nidhi Bhatia1, Narinder Pal Singh2
1Department of Anaesthesia and Intensive Care, Post Graduate Institute of Medical Education and Research, Sector-12, Chandigarh, India
2Department of Anaesthesia, MMIMSR, MM (DU), Mullana-Ambala, India
Abstract
Caesarean delivery is one of the commonest surgical procedures being performed world-wide, and with it comes the burden for management of acute post-operative pain in parturient. A number of modalities including neuraxial opioids, intravenous drugs and truncal nerve blocks are available to control acute postsurgical pain. Quadratus lumborum block has recently been emerged as a modality for pain relief following caesarean delivery. This review highlights the anatomical aspects, mechanism of action of block, relevant literature search and future directions for use of quadratus lumborum block in parturient undergoing caesarean delivery.
Pain after caesarean delivery
Caesarean delivery (CD) is the commonest surgical procedure performed worldwide. Adequately treated post caesarean pain allows early breastfeeding, enables the mother to take care of the new-born and helps in better maternal-neonatal bonding1. Management of post-delivery pain is thus one of the key determinants in improving perioperative care after CD2-4.
Poorly managed pain after CD can lead to postpartum depression (approximate incidence of 19%), reduced breast feeding success, delayed early ambulation with risk of thromboembolism and progression to persistent post-surgical pain2-5. The incidence of persistent post-caesarean pain has been found to be around 40% after three months and can last up to one year6,7. An ideal analgesic technique should not affect the mother’s ability to take care of a new-born and is minimally transferred via breast milk. None of the single technique (neuraxial opioids, paracetamol, NSAIDS, or nerve blocks) provides sufficient analgesia and is devoid of adverse effects. Hence multimodal analgesia has been advocated to control postoperative pain.
Multimodal techniques include neuraxial opioids, parenteral agents like opioids, paracetamol and NSAIDs. Intrathecal morphine remains the gold standard intraoperative intervention for controlling pain after CD8. Although being the standard of care and one of the oldest modalities for pain relief, central neuraxial blockade with intrathecal morphine (ITM) as an adjuvant, is associated with untoward side effects, like, pruritus, nausea, vomiting, and sedation9. Further, certain components of multimodal analgesics such as NSAIDS may be contradicted in patients having bleeding or renal impairment.
With widespread availability and increase in expertise with the use of ultrasound by anaesthesiologist, truncal plane blocks like transversus abdominis plane (TAP) block, quadratus lumborum block (QLB), erector spinae plane (ESP) block are being increasingly used for the management of pain in obstetric patients. TAP block has been shown to minimize analgesic requirement and decrease the pain scores in postoperative period. However, it does not provide extensive analgesia due to inadequate visceral coverage and analgesic effect is mainly dependent on the anatomical technique used10. On the other hand, ESP block provides both somatic and visceral analgesia, but it has not been extensively studied in post-CD scenario.
QLB is easy, safe and provides extensive analgesia from T7-L1 dermatomes due to the spread of drug injectate to paravertebral space11,12. Several randomized controlled trials and systematic reviews have recently been published to validate the role of QLB in managing acute pain in parturient following CD13-20.
In this narrative review, we provide an overview of anatomy, techniques and variants of QLB and outline the currently available data regarding its utility in women undergoing cesarean delivery.
Anatomy
QLB was first described by Blanco et al in 200721. QLB is a posterior abdominal wall block. Also known as interfascial plane block, it requires the local anaesthetic to deposit in the thoracolumbar fascia (TLF). TLF is a posterior extension of abdominal wall muscle fascia and engulfs the quadratus lumborum, psoas major and erector spinae muscles. Drug injected in this plane helps in preventing somatic and visceral pain after abdominal surgery22,23.
The more superficial nature of the block confers it with more safety and better resolution with use of ultrasound guidance. Due to the presence of quadratus lumborum muscle, the needle tip stays away from the peritoneum, hence reducing intraperitoneal injection and bowel injury. The precise mechanism of action of QLB has yet not been deciphered, but drug spread along TLF plays a significant role. Anatomically the TLF, is a sheet of fused aponeuroses, consists of anterior, middle and posterior layers. The anterior layer lies anterior to the quadratus muscle. Injectate is deposited between the anterior layer and the muscle, spreading cranially beneath the lateral arcuate ligament to endothoracic fascia. The drug might reach lower thoracic paravertebral space and thus accounts for visceral analgesia24. The middle layer flows between erector spinae muscles and quadratus lumborum muscle. The posterior layer of the TLF encloses the erector spinae muscle. (Figure I) The middle layer of the TLF connects the deep lamina of the posterior layer to the lateral border of erector spinae muscle. It forms a triangular area known as the lumbar interfascial triangle (LIFT), which is the main target site for drug injection in the QLB2. The LIFT is close to the thoracic paravertebral space, leading to drug spread in the paravertebral space and provides visceral analgesia22,23,25. Cadaveric studies reveal that direct spread of contrast into the roots and branches of the lumbar plexus can possibly lead to blockade of L1-L323,26,27. Blockade of sympathetic peripheral nerves can also be explained in a similar way. TLF has an extensive sensory network of both A and C nociceptors and mechanoreceptors, with sympathetic nerve fibres posterior to quadratus muscle and innervating TLF. Drug injected blocks these fibres and lead to changes in both local circulation and autonomic tone, enhance analgesic efficacy and reduce the incidence of both acute and chronic pain28,29.
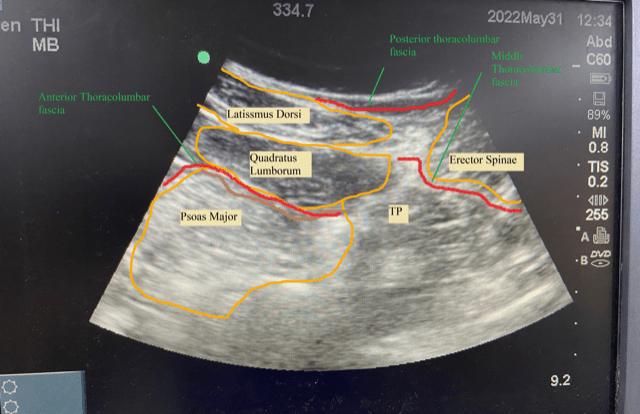
Figure 1: Anatomy of Quadratus Lumborum Block.
Numerous studies reported a longer duration of analgesia with QLB as compared to TAP block13-20. The most plausible explanation is the spread of the drug to the paravertebral space; this space is filled with adipose tissue. Since the perfusion in adipose tissue is low, absorption of anaesthetic into the systemic circulation is very slow leading to prolonged duration of action30.
Approaches of the block
The literature describes three different approaches to QLB, these are type 1 also known as lateral approach, type 2 or posterior approach and type 3 or transmuscular approach.
Technique of QLB
Block is preferably performed in the lateral decubitus position as it provides greater exposure to the neuraxial structures. Also, the position is more comfortable for performer as it provides better and firm grip of the ultrasound probe and needle. A low-frequency curved array probe is preferred as it allows visualization of lateral abdominal wall muscles and the quadratus lumborum muscle. The probe is initially placed in mid axillary line between the iliac crest and subcoastal margin and moved posteriorly, till tapering of three lateral abdominal muscles, and appearance of fascia transversalis and quadratus muscle is observed. At this time, the transverse process of the lumbar vertebra, erector spinae, psoas major and quadratus muscles can be acknowledged. (Figure II)
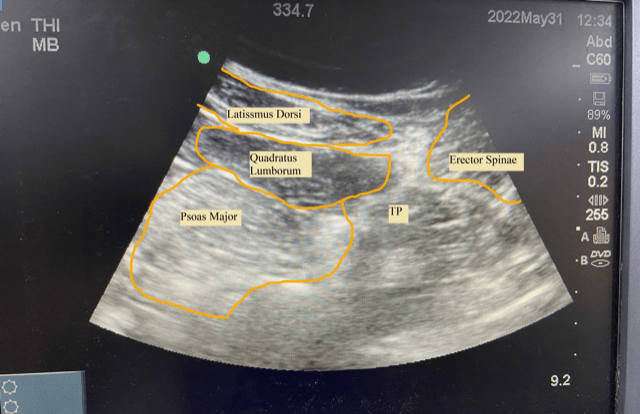
Figure 2: Sonoanatomy of Quadratus Lumborum Block (TP- Transverse process).
Needling Phase31,32,33
Type 1/lateral approach (Figure III)- In this approach, needle direction is from the mid axillary line towards the junction of tapered abdominal muscle layer and lateral border of QLM, The drug is deposited once the needle penetrates the transversus abdominis aponeurosis at the lateral border of QLM.
Type 2/posterior approach (Figure III)- In this approach, the direction of the needle is from the posterior axillary line to the posterior border of QLM. The local anaesthetic is deposited on the posterior surface of QLM, between QLM and erector spinae muscle.
Type 3/transmuscular approach (Figure III)- This is the most effective approach but necessitates the patient to be either in lateral or sitting position. The needle is directed from the posterior axillary line through erector spinae and QLM towards the anterior border of QLM. The drug is injected into the tissue plane between QLM and psoas muscle. This leads to the spread of the drug into thoracic paravertebral space and blocks lumbar nerve roots and somatic nerves, provides an extensive blockade from T6-T7 to L1-L2.
Type 4/Intramuscular approach- Herein the drug is injected directly into the quadratus muscle.
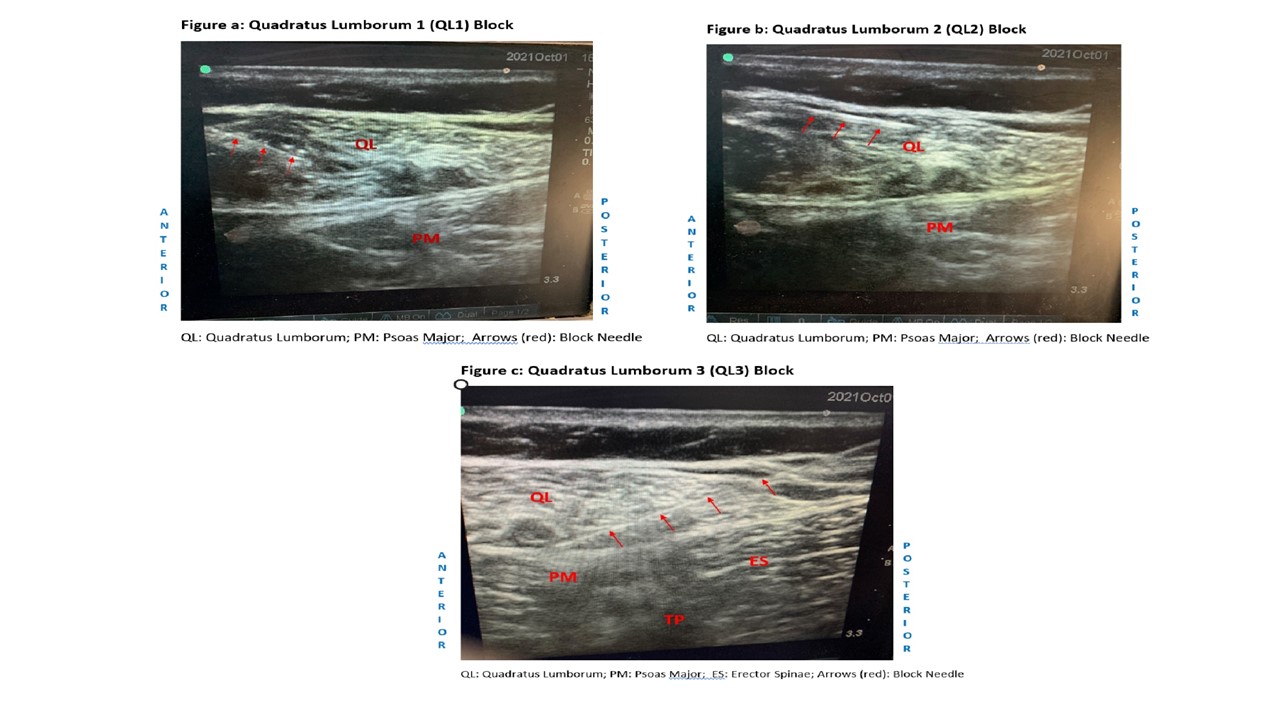
Figure 3: Anatomy and needle trajectory for a) Type 1 Quadratus Lumborum Block, b) Type 2 Quadratus Lumborum Block and c) Type 3 Quadratus Lumborum Block
Which approach should be preferred? There is limited literature on the safety and efficacy of the three techniques. The choice of the block depends upon the surgical anaesthesia desired and the expertise of the performer. Kang et al conducted a randomised trial to compare the effects of three QLB approaches (QLB type 2, QLB type 3, QLB type 2+3) and classic epidural analgesia (EA) for cesarean section under spinal anaesthesia. Authors reported lower pain scores and morphine consumption in QLB type 2+333. Cadaveric studies suggest the drug the drug spreads along transversus plane block in QLB1, along thoracolumbar fascia QLB2 and thoracic paravertebral space and into somatic and lumbar nerve roots in QLB329. Hence QLB3 appears to be most effective for analgesia purpose. However, QLB3 requires a steeper trajectory of the needle that too in a lateral position which appears to be difficult in a parturient following a CD19.
Dose and volume of Local Anaesthetic
As it is a plane block, a large volume of local anaesthetic is required for effective blockade. A volume of 20-30 ml is usually recommended. (0.2-0.4ml/kg of 0.2% to 0.5% ropivacaine or 0.1%-0.25% bupivacaine). In a parturient undergoing CD with a midline incision, a bilateral QLB should be given with limiting the drug dose.
Contraindications
Absolute contraindications include drug allergy to local anaesthetic, presence of acute infection at injectate site, sepsis, any coagulation abnormality or bleeding tendencies and patient refusal.
Relative contraindications include neurological disorder, hemodynamically unstable patient.
Complications
Although devoid of major complications due to the superficial nature of block, theoretical risks include the spread of local anaesthetic to lumbar plexus leading to weakness of psoas, iliacus and quadriceps muscle leading to delay in early ambulation34. Ueshima et al in a retrospective study reported an incidence of 15% of lower extremity weakness35. However, prospective trials or larger meta-analysis did not confirm these complications14,15,20.
It can lead to hypotension because of the spread of drug in the bilateral paravertebral spaces36. There is also a potential risk of hematoma formation due to manipulation of the fascia at the level of exit of blood vessels from paravertebral space14. Local anaesthetic toxicity (LAST) can occur due to large volume of LA, which can be more pronounced in the pregnant female. Increased cardiac output, faster perfusion at the injection site and reduced alpha 1 acid glycoprotein causing less bound LA, leads to increased concentration of LA into the systemic circulation and higher peak concentrations in parturient37,38. There is a paucity of large-scale studies to decipher the incidence of LAST in parturient receiving various abdominal plane blocks37,38.
The efficacy of QLB has been elicited through several randomized trials and the block has been in clinical use in post-caesarean pain since its inception13-20. Blanco et al had randomized 796 parturient undergoing CD to receive TAP or QLB and found that QLB is superior to TAP block. Authors reported significantly lower morphine consumption at various time intervals up to 48 hours in patients receiving QLB. Authors could not appreciate any significant difference in VAS scores among the two groups at different time points at rest or with movement. They concluded, QLB to be more effective in reducing postoperative morphine consumption compared to TAP block after CD with effects lasting till 48 hours14.
In a recent meta-analysis by Singh et al, authors assessed the analgesic potential of QLB in women undergoing CD19. The primary outcome was 24 hour opioid consumption in the postoperative period. Secondary objectives were opioid consumption at 48 hours, pain scores at varied time points and side effects. Seven trials meeting the eligibility criteria were included. There was a significant reduction in opioid consumption in QLB compared to control or sham in patients. The mean difference in parenteral morphine consumption in 24 hours was reported to be 9.93 mg (95%CI -11.47 to -8.38) in patients receiving QLB along with spinal anaesthesia without ITM. However, QLB did not provide any added analgesic benefit to patients who received ITM. Further, QLB significantly reduced pain scores both at rest and movement up to 24 hrs19.
In a network meta-analysis conducted by Boghdadly et al, authors compared TAP block and QLB with each other and with control with or without ITM20. A total of 31 trials met inclusion criteria and a total of 2188 patients were included. The primary outcome was cumulative intravenous morphine equivalent consumption 24 hours postoperatively. Authors reported that the analgesic efficacy of TAP and QLB were equivalent and both were superior to control when used in absence of ITM. However, in presence of ITM neither of the two blocks could significantly reduce the morphine consumption in comparison to control. Most RCTs evaluated lateral or posterior QLB, which is usually associated with lesser paravertebral space spread and hence less analgesic profiles. Also, QLB was found to be inferior to TAP and control groups in terms of time to ambulation. The authors concluded that both QLB and TAP block were comparable and superior to control in absence of ITM.
QLB has been used as a modality for pain relief in many other surgeries with promising results for postoperative pain management. It has been used for lower abdominal procedures, laparoscopic cholecystectomy, laparoscopic colorectal surgeries, laparoscopic inguinal hernia repairs39,40. It has been used for gynaecological procedures like total abdominal hysterectomy41, extracorporeal shock wave lithotripsy42,43, orthopaedic surgeries44,45,46 and also has been used in paediatric surgeries like, orchidopexy, lower abdominal surgeries and inguinal hernia repair47,48.
Future research
Future research should focus on efficacy of different approaches of QLB in isolation or their combinations; the role of various additives and catheter-based techniques. Researchers should also specifically seek the data on block-related complications. Although safe, QLB is a technically difficult block as the needle moves closer to abdominal and retroperitoneal structures and requires vigilance. QLB has a promising role in multimodal analgesic regimens following CD.
References
- Sultan P, Sharawi N, Blake L, et al. Enhanced recovery after caesarean delivery versus standard care studies: a systematic review of interventions and outcomes. Int J Obstet Anesth. 2020; 43: 72-86.
- Wilson RD, Caughey AB, Wood SL, et al. Guidelines for antenatal and preoperative care in cesarean delivery: enhanced recovery after surgery society recommendations (part 1). Am J Obstet Gynecol. 2018; 219: 523-32.
- Caughey AB, Wood SL, Macones GA, et al. Guidelines for intraoperative care in cesarean delivery: enhanced recovery after surgery society recommendations (part 2). Am J Obstet Gynecol. 2018; 219: 533-44.
- Macones GA, Caughey AB, Wood SL, et al. Guidelines for postoperative care in cesarean delivery: enhanced recovery after surgery (ERAS) society recommendations (part 3). Am J Obstet Gynecol. 2019; 221: 247.
- Lavand’homme P. Postcesarean analgesia: effective strategies and association with chronic pain. Curr Opin Anaesthesiol. 2006; 19: 244-248.
- Lavand’homme P. Chronic pain after childbirth. Curr Opin Anaesthesiol. 2013; 26: 273-277.
- Kainu JP, Sarvela J, Tiippana E, et al. Persistent pain after caesarean section and vaginal birth: a cohort study. Int J Obstet Anesth. 2010; 19: 4-9.
- National Institute for Health and Care Excellence. Caesarean Section. NICE. CG132. Caesarean section. 2019. https://www. nice.org.uk/guidance/cg132 (accessed 16/07/2020)
- Apfelbaum JL, Hawkins JL, Agarkar M, et al. Practice guidelines for obstetric anesthesia: an updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology 2016; 124: 270-300.
- Champaneria R, Shah L, Wilson MJ, et al. Clinical effectiveness of transversus abdominis plane (TAP) blocks for pain relief after cesarean section: a meta-analysis. Int J Obstet Anesth. 2016; 28: 45-60.
- Chin KJ, McDonnell JG, Carvalho B, et al. Essentials of our current understanding: Abdominal wall blocks. Reg Anesth Pain Med. 2019; 42: 133-183.
- Mitchell KD, Smith CT, Mechling C, et al. A review of peripheral nerve blocks for cesarean delivery analgesia. Reg Anesth Pain Med. 2019.
- Blanco R, Ansari T, Girgis E. Quadratus lumborum block for postoperative pain after caesarean section: a randomised controlleds trial. Eur J Anaesthesiol. 2015; 32: 812-818.
- Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016; 41: 757-62.
- Hansen CK, Dam M, Steingrimsdottir GE, et al. Ultrasound guided transmuscular quadratus lumborum block for elective cesarean section significantly reduces postoperative opioid consumption and prolongs time to first opioid request: a double-blind randomized trial. Reg Anesth Pain Med. 2019; 44: 896-900.
- Irwin R, Stanescu S, Buzaianu C, et al. Quadratus lumborum block for analgesia after caesarean section: a randomised controlled trial. Anaesthesia. 2020; 75: 89-95.
- Krohg A, Ullensvang K, Rosseland LA, et al. The analgesic effect of ultrasound-guided quadratus lumborum block after cesarean delivery. Anesth Analg. 2018; 126: 559-65.
- Mieszkowski MM, Mayzner-Zawadzka E, Tuyakov B, et al. Evaluation of the effectiveness of the Quadratus Lumborum Block type I using ropivacaine in postoperative analgesia after a cesarean section - a controlled clinical study. Ginekologia Polska. 2018; 89: 89-96.
- Singh NP, Makkar JK, Borle A, et al. The analgesic efficacy of quadratus lumborum block in caesarean delivery: a meta-analysis and trial sequential analysis. Journal of Anesthesia. 2020; 34: 814-24.
- Boghdadly K, Desai N, Halpern S, et al. Quadratus lumborum block vs transversus abdominis plane block for caesarean delivery: a systematic review and network meta-analysis. Anaesthesia. 2021; 76: 393-403.
- Blanco R. TAP block under ultrasound guidance: the description of a ‘non pops technique’. Reg Anesth Pain Med. 2007; 32: 130.
- Schuenke MD, Vleeming A, Van Hoof T, et al. A description of the lumbar interfascial triangle and its relation with the lateral raphe: anatomical constituents of load transfer through the lateral margin of the thoracolumbar fascia. J Anat. 2012; 221: 568-576.
- Willard FH, Vleeming A, Schuenke MD, et al. The thoracolumbar fascia: anatomy, function and clinical considerations. J Anat. 2012; 221: 507-536.
- Tamura T, Kitamura K, Yokota S, et al. Spread of Quadratus Lumborum Block to the Paravertebral Space Via Intramuscular Injection: A Volunteer Study. Reg Anesth Pain Med. 2018; 43: 372-7.
- Blanco R. Optimal point of injection: the quadratus lumborum type I and II blocks. Anesthesia. 2013; 68: 4.
- Elsharkawy H, El-Boghdadly K, Kolli S, et al. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block. Eur J Anaesthesiol. 2017; 34: 587-95.
- Saito T, Den S, Tanuma K, et al. Anatomical bases for paravertebral anesthetic block: fluid communication between the thoracic and lumbar paravertebral regions. Surg Radiol Anat. 1999; 21: 359-63.
- Dam M, Hansen CK, Børglum J, et al. A transverse oblique approach to the transmuscular quadratus lumborum block. Anaesthesia. 2016; 71: 603-4.
- Carline L, McLeod GA, Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth. 2016; 117: 387-94.
- Thomas JM, Schug SA. Recent advances in the pharmacokinetics of local anaesthetics. Long-acting amide enantiomers and continuous infusions. Clin Pharmacokinet. 1999; 36: 67-83.
- Elsharkawy H, El-Boghdadly K, Kolli S, et al. Injectate spread following anterior subcostal and posterior approaches to the quadratus lumborum block: a comparative cadaveric study. Eur J Anaesthesiol. 2017; 34: 587-95.
- Ueshima H, Otake H, Lin JA. Ultrasound-Guided quadratus lumborum block: an updated review of anatomy and techniques. Biomed Res Int. 2017; 2017: 1-7.
- Kang W, Lu D, Yang X, et al. Postoperative analgesic effects of various quadratus lumborum block approaches following cesarean section: a randomized controlled trial. J Pain Res. 2019; 12: 2305-2312.
- Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia. 2017; 72: 230-2.
- Ueshima H, Hiroshi O. Incidence of lower-extremity muscle weakness after quadratus lumborum block. J Clin Anesth. 2018; 44: 104.
- Sá M, Cardoso JM, Reis H, et al. Quadratus lumborum block: are we aware of its side effects? A report of 2 cases. Rev Bras Anestesiol. 2017; 68: 396-9.
- Gitman M, Barrington MJ. Local anesthetic systemic toxicity: a review of recent case reports and registries. Reg Anesth Pain Med. 2018; 43: 124-30.
- El-Boghdadly K, Pawa A, Chin KJ. Local anesthetic systemic toxicity: current perspectives. Local Reg Anesth. 2018; 11: 35-44.
- Kadam VR. Ultrasound-guided quadratus lumborum block as a postoperative analgesic technique for laparotomy. J Anaesthesiol Clin Pharmacol. 2013; 29: 550-2.
- Ueshima H, Hiroshi O. Intermittent bilateral anterior subcostal quadratus lumborum block for effective analgesia in lower abdominal surgery. J Clin Anesth. 2017; 43: 65.
- Ishio J, Komasawa N, Kido H, et al. Evaluation of ultrasound-guided posterior quadratus lumborum block for postoperative analgesia after laparoscopic gynecologic surgery. J Clin Anesth. 2017; 41: 1-4.
- Corso RM, Piraccini E, Sorbello M, et al. Ultrasound-guided transmuscular quadratus lumborum block for perioperative analgesia in open nephrectomy. Minerva Anestesiol. 2017; 83: 1334-5.
- Ueshima H, Otake H. Clinical experiences of unilateral anterior sub-costal quadratus lumborum block for a nephrectomy. J Clin Anesth. 2018; 44: 120.
- Ueshima H, Yoshiyama S, Otake H. The ultrasound-guided continuous transmuscular quadratus lumborum block is an effective analgesia for total hip arthroplasty. J Clin Anesth. 2016; 31: 35.
- Johnston DF, Sondekoppam RV. Continuous quadratus lumborum block analgesia for total hip arthroplasty revision. J Clin Anesth. 2016; 35: 235-7.
- Sondekoppam RV, Ip V, Johnston DF, et al. Ultrasound-guided lateral-medial transmuscular quadratus lumborum block for analgesia following anterior iliac crest bone graft harvesting: a clinical and anatomical study. Can J Anaesth. 2018; 65: 178-87.
- Hernandez MA, Vecchione T, Boretsky K. Dermatomal spread following posterior transversus abdominis plane block in pediatric patients: our initial experience. Paediatr Anaesth. 2017; 27: 300-4.
- Aksu C, Gürkan Y. Ultrasound guided quadratus lumborum block for postoperative analgesia in pediatric ambulatory inguinal hernia repair. J Clin Anesth. 2018; 46: 77-8.
