Assessment and Management of Difficult Airway Post Mandibulectomy: A Narrative Review
Swati Patel, Ashwini Reddy, Amiya Kumar Barik*, Shiv Lal Soni, Narender Kaloria
Department of Anaesthesia and Intensive Care, Post Graduate Institute of Medical Education and Research, Chandigarh, India
Abstract
Mandibulectomy most commonly performed as surgical management of oropharyngeal carcinoma leads to a wide array of anatomical and physiological changes which result in an anticipated difficult airway. There may be posterosuperior displacement of hyoid bone and tongue leading to reduction of retropalatal space along with loss of structural support to the tongue predisposing it to prolapse and development of obstructive sleep apnoea. Bulky flap reconstruction, limited mouth opening, and radiotherapy limiting neck mobility further compound the difficulty in airway management. This leads to a wide spectrum of issues ranging from difficulty in face mask ventilation to laryngoscopy and intubation. It is essential to individualize each case with a preformulated strategy outlining the primary and alternative approaches. A literature search was carried out using search engines like PubMed, Embase, Medline, and Google scholar using the terms “Difficult airway”, “Post-mandibulectomy”, “Difficult laryngoscopy, and Intubation”. The available literature was thoroughly reviewed by the authors before the final drafting of this article. A multidisciplinary team approach, thorough assessment, meticulous preparation, and critical decision-making are essential for successfully managing a difficult airway post-mandibulectomy.
Introduction
Mandibular defects may be secondary to congenital or acquired pathology like trauma and surgical management of oral cancer ultimately leading to functional disability and aesthetic deformities, according to the location and size of the segmental defect. Mandibular surgery results in a reduction in the hypopharyngeal and retro-lingual space.1 A decrease in the retro-lingual airway space by 12.8 % in volume and 28 % in distance post mandibular setback surgery was reported by Tselnik and Pogrel.2 It was also reported by Wickwire et al. that mandibular surgery causes a posterosuperior shift of the hyoid bone leading to the displacement of the tongue in a similar vector which then comes into contact and displaces the soft palate backward and upwards.3 These factors ultimately lead to the narrowing of the retropalatal airway and also contribute to the development of obstructive sleep apnoea (OSA), particularly in the absence of a flap or rigid reconstruction of the lower jaw.4 The loss of tongue musculature and structural support of the tongue leading to prolapse may also compromise the airway. Pathologic changes such as fibrosis, vascular engorgement, inflammatory cell infiltration, and edema further contribute to airway obstruction.5 Difficulty in mastication and deglutition secondary to bone and muscular atrophy of the mandible may also lead to nutritional deficiencies and long-term functional disability.
Difficulty or failure to manage challenging airways results in airway trauma, dental injury, hypoxic brain damage, or even death. The Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society revealed that severe adverse airway management events like emergency surgical airway, hypoxic brain damage, or death were seen in 1 of every 22,000 tracheal intubation cases.6 The number of unreported events is expected to be much higher. It is thus essential to remain vigilant during airway management. This review article provides an overview of the definition, incidence, assessment, and management of an anticipated difficult airway due to prior mandibulectomy in the operating room.
Definition and incidence of the difficult airway
The term “difficult airway” covers an array of issues ranging involving difficulty in ventilation with bag and mask ventilation or supraglottic airway insertion to encountering difficulty in tracheal intubation or gaining front-of-neck access. The American Society of Anaesthesiologists guidelines in 2022 described a difficult airway as the clinical situation in which anticipated or unanticipated difficulty or failure is experienced by a physician trained in anesthesia care, including but not limited to one or more of the following: face-mask ventilation, laryngoscopy, ventilation using a supraglottic airway, tracheal intubation, extubation, or invasive airway.7 Canadian guidelines are broader, defining the difficult airway as an airway for which an experienced practitioner anticipates or encounters difficulty with facemask ventilation, tracheal intubation using direct or indirect laryngoscopy, or supraglottic airway use or recognizes the need for an emergency surgical airway.8 Various studies have reported that the incidence of difficult face mask ventilation ranges from 1.4 to 5.0%, and impossible face mask ventilation ranges from 0.07 to 0.16%.9,10 Difficult tracheal intubation is seen in 5 to 8% of cases and the incidence of failed tracheal intubation ranges from 0.05 to 0.35%.11
Preoperative evaluation
A complete airway assessment includes a bedside screening examination along with a review of physiological and anatomical features, that may influence the plan of management of the airway. Hence, a thorough preoperative screening of the patient including assessment of comorbidities and related medication is essential.12 A detailed history of prior surgery, the type of flap reconstruction performed, and a history of the previous tracheostomy should be elicited. The tumor locations in the oral cavity, pharynx, larynx, etc causing difficulty in deglutition results in nutritional disorders associated with weight loss, anemia, and electrolyte imbalance which must also be investigated accordingly.13 History of chemotherapeutic agents with adverse systemic side effects and radiotherapy leading to anatomical changes in the airway including fibrosis and restriction of neck extension is also crucial. The movement of vocal cords and the presence of any nerve palsy should also be evaluated.14 Anterior mandibulectomy additionally predisposes to the development of OSA which should also be assessed. Additionally, patients presenting with oropharyngeal carcinoma are often older, thus increasing the difficulty in airway management due to pathophysiological and anatomic changes that occur with aging.15 Factors predicting a difficult airway can broadly be divided into physiological, anatomical, or contextual categories (Table 1). It is also necessary to inform the patient/patient’s kin of the risk involved and any distinct procedures related to difficult airway management.
Table 1: Factors predicting a difficult airway post mandibulectomy11
|
Anatomical Factors |
|
|
Difficulty face-mask ventilation |
Large mandibular defect |
|
Perioral/ peri-glottic growth |
|
|
Bulky flap reconstruction |
|
|
Posterosuperior displacement of tongue |
|
|
Lack of teeth |
|
|
History of neck irradiation |
|
|
History of OSA |
|
|
Obesity |
|
|
Modified Mallampati class ¾ |
|
|
Difficulty Laryngoscopy and Intubation |
Limited mouth opening |
|
Tumour extension till base of the tongue |
|
|
Bulky flap reconstruction |
|
|
Limited neck extension |
|
|
Decreased thyromental distance |
|
|
Decreased sterno-mental distance |
|
|
Poor submandibular compliance |
|
|
Peri-pharyngeal growth |
|
|
Cormack-Lehane grade ¾ |
|
|
Difficult SGA insertion |
Limited mouth opening |
|
Obstructing lesion in the upper airway |
|
|
Limited neck mobility |
|
|
Large mandibular defect leading to dislodgement |
|
|
Physiological factors |
Obstructive sleep apnoea |
|
Obesity |
|
|
Hemodynamic instability |
|
|
Contextual factors |
Experience and skills of attending anesthesiologist |
|
Availability of Equipment |
|
|
Patient cooperation |
|
|
Urgency of situation |
|
|
Availability of skilled help |
The most common bedside screening tests for assessment of the airway include degree of mouth opening, thyromental distance, the modified Mallampati test (MMP) grade, sterno-mental distance, upper lip bite test, or any combination of these tests. A Cochrane systematic review of data from 133 studies including 844,206 participants studied the seven most common screening tests for difficult airway assessment i.e Mallampati test, MMP test, mouth opening test, Wilson risk score, sternomental distance, thyromental distance, upper lip bite test and concluded that none of these tests (alone or in combination), were well suited for the detection of an unanticipated difficult airway. They found that difficult laryngoscopy was best diagnosed by the upper lip bite test which had the highest sensitivity (P < 0.001) and difficult tracheal intubation was best diagnosed by the modified Mallampati test (P < 0.001).16
Upper airway ultrasonography is an emerging tool that has proved itself invaluable during airway assessment, procedural interventions, and decreasing the rate of airway-related complications. Gomes et al. conducted a meta-analysis that studied the use of airway ultrasound to predict the incidence of difficult laryngoscopy and difficult intubation in 5000 patients who underwent elective surgeries under general anesthesia. This study suggested that the use of hyomental distance in the neutral position is the most reliable parameter for pre-operative airway ultrasound assessment and can help anesthetists in airway preparation properly and for a better patient safety profile.17 Hyomental distance is invariably reduced in patients who have undergone mandibulectomy. A systemic review conducted by Vaquero et al. highlighted the importance of the use of preoperative airway ultrasound to screen out difficult airway cases. They found out that the distance from skin to epiglottis in the sniffing position is the most reliable parameter for preoperative airway ultrasound and can be considered as an independent predictor for direct difficult laryngoscopy.18
Intraoperative Management
Airway examination is only one facet of management of the difficult airway. The other aspects are the availability of technical equipment and experienced operators. Meticulous preparation of the operation theatre with the required drugs and equipment is essential. Difficult airway cart comprising face masks of different sizes, laryngoscopes with a selection of blades, stylets, endotracheal tubes of all sizes, nasopharyngeal and oropharyngeal airways, SGAD, video laryngoscopes, flexible bougies, a cricothyroid puncture kit, suction, rigid optic laryngoscopes, and fibreoptic should be kept ready.19 A well-informed team with appropriate distribution of roles following a structured approach is essential for the safe conduct of anesthesia and securing an anticipated difficult airway. This preformulated approach is subject to the state of the patient, the expected surgery, and the preferences and skills of the attending anesthesiologist.8 Various recommendations and algorithms to provide an organized pathway to secure a difficult airway have been proposed by many expert international bodies, but none of these pathways includes all clinical situations, and none of them are without risk.6,7,8,12 It is thus crucial to individualize each patient and formulate a definitive plan and alternative approaches as well (Table 2 & Table 3).
Table 2: Airway management and Rescue techniques options in post mandibulectomy patients based on ASA, DAS guidelines:
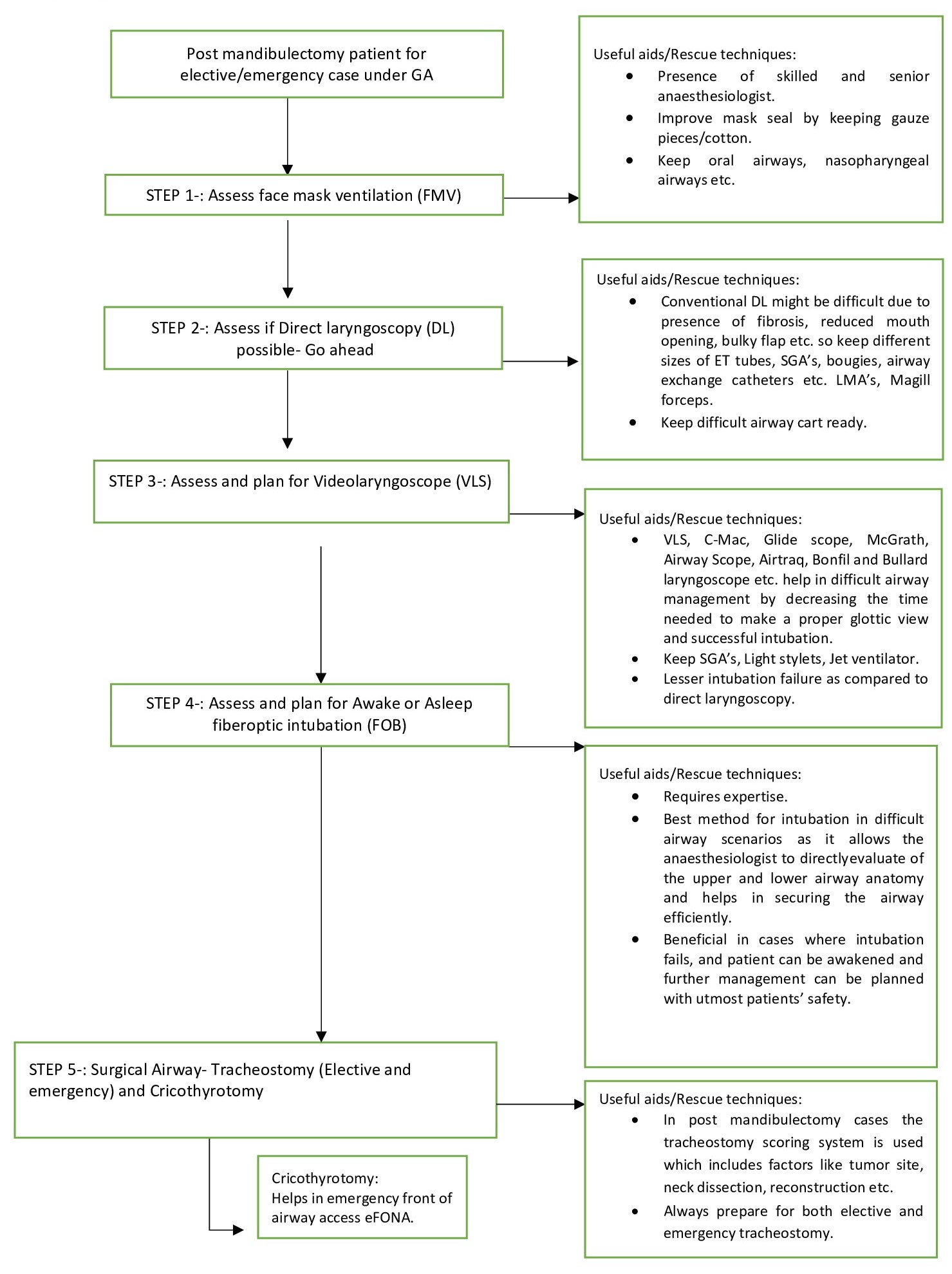
Table 3: Summary of ASA 2022 difficult airway guidelines with literature review and recommendations and statistically significant outcomes (P < 0.01) are designated as either beneficial (B) or harmful (H); statistically nonsignificant findings are designated as equivocal (E).
|
Category |
Level |
Evidence based on |
Recommendation |
|
A |
1 |
Meta-analysis of randomized controlled trials (RCT)
|
1. Improved laryngeal views, a higher frequency of successful intubations, a higher frequency of first attempt intubations, and fewer intubation maneuvers with video-assisted laryngoscopy and findings for time to intubation were equivocal. (Category A1-B evidence) |
|
|
2 |
Multiple randomized controlled trials |
1. Video-assisted laryngoscopy with awake laryngoscopy with a flexible intubation scope reported equivocal findings for laryngeal view, visualization time, first attempt intubation success, and time to intubation. (Category A2-E evidence) 2. Laryngoscopic view, intubation success, first attempt intubation success, and time to intubation when hyperangulated videolaryngoscopes (VLS) were compared with nonangulated VLS for anticipated difficult airways. (Category A2-E evidence) 3. Flexible intubation through supraglottic airways (SGA) versus flexible intubation scopes alone reported a higher frequency of first attempt intubation success with the SGA. (Category A2-B evidence) 4. Second generation SGA with first generation SGA reported faster times to intubation with second generation SGA. (Category A2-B evidence) 5. Shorter intubation times when lighted stylets were compared with direct laryngoscopy (DL). (Category A2-B evidence) |
|
|
3 |
A single RCT
|
1. The ramped with sniffing positions reported equivocal findings for laryngoscopic view and intubation success. (Category A3-E evidence) 2. Levering laryngoscopes to standard laryngoscopes reported no differences in laryngoscopic view, but shorter times to intubation and fewer intubation maneuvers were needed for successful intubation with the levering laryngoscope. (Category A3-B evidence) 3. Channel-guided VLS with non–channel-guided VLS reported equivocal findings for laryngeal view, intubation success, first attempt intubation, time to intubation, and needed intubation maneuvers. (Category A3-E evidence) 4. Intubation with a lightwand versus blind intubation for patients with anticipated difficult airways reported a significantly higher frequency of successful intubations and shorter. (Category A3-E evidence) 5. VLS combined with a flexible bronchoscope reported a greater first attempt success rate with the combination technique than with a VLS alone. (Category A3-B evidence) |
|
B |
1 |
Nonrandomized studies with group comparisons; |
1. VLS with DL reported equivocal findings for intubation success with difficult airways in emergency. (Category B1-E evidence) 2. In comparison of successfully extubated patients with patients who failed extubation observed differences in duration of intubation; conditions associated with failed extubation included airway granulations and subglottic stenosis. (Category B1-H evidence) |
|
|
2 |
Nonrandomized studies with associative findings |
1. Findings for facial and jaw features anatomical measurements, and ultrasound anatomical measurement were shown to have very high predictive and comparative variability, with sensitivity, specificity, and significance values ranging from low to very high across all difficult vs nondifficult airway patient. (Category B2-E evidence) 2. Improved laryngeal views (during tongue protrusion) when transnasal endoscopy was added to the preoperative bedside evaluation. (Category B2-B evidence) 3. Comparison of the sniffing position with head and neck raised beyond the sniffing position reported improved laryngeal views with the raised position. (Category B-2 B evidence) 4. Intubation with a flexible bronchoscope versus DL reported equivocal findings for complicated intubations. (Category B2-E evidence) |
|
|
3 |
Nonrandom- ized studies with descriptive findings |
1. Utilizing preoperative endoscopic examination as an added airway assessment tool reported that airway management plans were revised in 26% of patients. (Category B3-B evidence) 2. Radiography and CT scans identified anatomical characteristics such as laryngeal deviations, cervical abnormalities, fractures, and abscesses that may suggest a potential difficult airway. (Category B3-B and B4-B evidence) 3. Patient questionnaires may identify patients at risk of difficult ventilation and intubation. (Category B3-B evidence) 4. Successful awake intubation in 88 to 100% of anticipated difficult airway patients. (Category B3-B evidence) 5. Intubation success ranging from 87 to 100% of patients. (Category B3-B evidence) 6. Intubation success rates for VLS ranging from 85 to 100% of patients and first attempt successful intubation rates ranging from 51 to 100%. (Category B3-B evidence) 7. Flexible intubation scopes indicated success rates ranging from 78 to 100%. (Category B3-B evidence) 8. Successful SGA insertion and intubation ranging from 65 to 100% of anticipated difficult airway patients. (Category B3-B evidence) 9. Oxygen desaturation occurring in 1.8 to 3.3% of patients after supraglottic airway placement. (Category B3-H evidence) 10. Successful intubation ranging from 84.9 to 100% of anticipated difficult airway patients when lighted stylets were used. (Category B3-B evidence) 11. Successful intubation with combination techniques ranging from 80 to 90% and first attempt success rates ranging from 50 to 100% of anticipated difficult airway patients. (Category B3-B evidence) 12. Successful percutaneous tracheostomy for an anticipated difficult airway patient as an alternative after unsuccessful surgical tracheostomy. (Category B3-B evidence) 13. First attempt intubation success rate for difficult airways of 96% with bougies and 82% with stylets and tracheal tubes in an emergency department. (Category B3-B evidence) 14. Flexible bronchoscopy success rate of 78% for intubation rescue after failed direct laryngoscopy. (Category B3-B evidence) 15. A 78% successful rescue intubation rate, and 94.1% successful rescue ventilation with SGA placement. (Category B3-B evidence) 16. A success rate with a lighted stylet of 77% for intubation rescue after failed direct laryngoscopy. (Category B3-B evidence) 17. Successful intubation in 97.7%, first attempt success in 86.4%, and successful ventilation in 100% of unanticipated difficult airway patients using a combination of a SGA and lighted stylet. (Category B3-B evidence) 18. Success rate with a lighted stylet of 77% for intubation rescue after failed direct laryngoscopy. (Category B3-B evidence) 19. Successful intubation in 97.7%, first attempt success in 86.4%, and successful ventilation in 100% of unanticipated difficult airway patients using a combination of a SGA and lighted stylet. (Category B3-B evidence) 20. Comparing percutaneous dilatational tracheotomy with percutaneous cricothyrotomy reported successful procedure rates of 97.6 and 95.3%. (Category B3-B evidence) 21. Restoration of oxygen saturation levels to above 90% when rescue transtracheal jet ventilation was used is advised. (Category B3-B evidence) 22. Staged extubation and reintubation with a Cook airway exchange catheter was successful in 92% of known or presumed difficult extubation patients. (Category B3-B evidence) 23. Successful extubation with an airway exchange catheter. (Category B3-B evidence) 24. Case report observed an esophageal misplacement of an airway exchange catheter during extubation of a diffIcult airway patient. (Category B3-H evidence) |
|
|
4 |
Case series or Case reports |
1. Difficult laryngoscopy or difficult intubation occurring among patients with a variety of acquired or congenital disease states (e.g., ankylosing spondylitis, degenerative osteoarthritis, Treacher–Collins, Klippel–Feil, Down syndrome, mucopolysaccharidosis, and airway masses). (Category B4-H evidence) 2. Awake intubation (e.g., blind tracheal intubation, intubation through supraglottic devices, optically guided intubation) also observed success with anticipated difficult airway patients. (Category B4-B evidence) 3. Use of a backward-upward-rightward pressure of the larynx maneuver resulted in successful intubation of difficult airway patients. (Category B4-B evidence) 4. Successful intubation using external cricoid manipulation after failed direct intubation. (Category B4-B evidence) 5. Intubation success with levering laryngoscopic blades. (Category B4-B evidence) 6. Mechanical failure and arytenoid dislocation have been noted with levering blades. (Category B4-H evidence) 7. Intubation success with bougies and stylets. (Category B4-B evidence) 8. VLS intubation successes with a wide range of difficult airway conditions. (Category B4-B evidence) 9. Successful intubation with flexible intubation scopes. (Category B4-B evidence) 10. Successful ventilation and intubation with various supraglottic airways. (Category B4-B evidence) 11. Successful intubations when retrograde wire–graded intubation was performed for patients with anticipated difficult airways. (Category B4-B evidence) 12. Successful emergency ventilation via tube exchangers using expiratory ventilation assistance after multiple failed intubation attempts. (Category B4-B evidence) 13. Intubation successes with bougies, introducers, and stylets for patients with unanticipated or emergency difficult airways. (Category B4-B evidence) 14. Successful VLS guided intubation rates after failed intubation ranging from 92 to 100% for unanticipated and emergency difficult airways. (Category B4-B evidence) 15. Successful intubation with videolaryngoscopes in unantictipated and emergency difficult airways. (Category B4-B evidence) 16. Flexible bronchoscopy or fiberoptic nasotracheal intubation observed successful rescue intubations for unanticipated and emergency difficult airways. (Category B4-B evidence) 17. Successful rescue ventilation and intubation using supraglottic airways for unanticipated and emergency difficult airways. (Category B4-B evidence) 18. Case reports observed successful intubations with lighted stylets after failed direct laryngoscopies for emergency airways. (Category B4-B evidence) 19. Successful intubation with a rigid bronchoscope in an emergency airway obstruction case. (Category B4-B evidence) 20. Intubation success for unanticipated and emergency airway patients when combination techniques were used. (Category B4-B evidence) 21. A case series of two patients reported successful intubation using retrograde wire–guided intubation after failed intubation through a supraglottic airway. (Category B4-B evidence) 22. Improvements in oxygen saturation levels with supraglottic jet oxygenation in “cannot intubate, cannot ventilate” situations. (Category B4-B evidence) 23. Oxygen saturations of 72 to 100% with the use of ECMO for difficult airways before intubation attempts for emergency procedures. (Category B4-B evidence) |
In post-surgical patients of mandibulectomy, there is a battery of problems that make airway management crucial and challenging like restricted mouth opening, presence of residual tumor growth in the oral -cavity affecting the airway patency, decreased neck movement, tissue fibrosis, presence of trismus, post-surgery localized edema in the airway, increased chances of bleeding and aspiration etc. These concerns focus on ensuring proper detailed airway management planning and preparing the rescue techniques.5 The first step is to ensure adequate preoxygenation before manipulation of the airway as a rule and endeavour to provide supplemental oxygen via nasal cannula, facemask, laryngeal mask airway, or insufflation throughout the process till the airway is secured.7,8
Difficult face-mask ventilation
Face-mask ventilation (FMV) is the first step and a fundamental aspect of the maintenance of oxygenation. In post-mandibulectomy patients, the mandibular defect makes FMV difficult, so placing gauze pieces or cotton to fill the defect and maintaining a proper oxygenation seal might be helpful.20 FMV is also used as the rescue maneuver between two failed attempts at intubation of the trachea or insertion of the supraglottic airway (SGA). Adequate chest rises, square waveform capnography tracing, and adequate oxygen saturation confirm effective ventilation. Oropharyngeal or nasopharyngeal airways are effective aids and adjunctive maneuvers like chin-lift and jaw thrust are also used to maintain patency of the airway.20 The neuromuscular blockade is also said to improve mask ventilation. However, in post-mandibulectomy patients, the nasopharyngeal airway is preferred and jaw thrust and chin lift have limited efficacy depending on the size of the defect. Achieving an effective face mask seal is also challenging. It is also important to limit airway pressures during bag and mask ventilation to less than 30 cm H2O in case of friable oropharyngeal mass. A residual peri-glottic or perioral growth renders bag and mask ventilation difficult to impossible.
Difficult laryngoscopy and tracheal intubation
Undiagnosed tumor extension to the tongue base leading to tongue fixation causes difficulty in laryngoscopy and intubation. Decreased inter incisor gap due to anatomical changes, fibrosis or bulky flap reconstruction leads to difficulty in introducing a laryngoscope into the oral cavity. Limited neck mobility secondary to radiotherapy also contributes to difficult intubation.21
Difficult tracheal intubation does not equate to difficult laryngoscopy. A poorly visualized larynx (Cormack–Lehane grade 3/4) is not suggestive of difficult intubation of the trachea, particularly if adjuncts like a stylet are used.11 Successive attempts should be undertaken using either an alternative device like a video laryngoscope/ flexible bronchoscope or after the change of operator or optimizing the patient’s head and neck positioning. Visualization of the larynx can also be improved sometimes by increasing the depth of anesthesia and neuromuscular blockade.8,9
Multiple attempts of intubation also increase the chance of bleeding from the friable residual tumor mass. Two additional optimized efforts at intubation of the trachea can be taken before considering an alternative approach. Hasegawa et al. studied the incidence of adverse events during intubation in a multicentre study of 2616 patients and found that multiple attempts at tracheal intubation (>2) were independently related to increased incidence of adverse events like dysrhythmia, cardiac arrest, hypoxemia, airway trauma, and regurgitation.22
Video laryngoscopy is a valid alternative for further attempts. The Canadian Airway Focus Group also recommends it as the first choice for anticipated difficult tracheal intubation.8 The overall success rate for video laryngoscopy-assisted tracheal intubation is often higher than for direct laryngoscopy. A recent Cochrane review published in 2022 which studied 26149 adult participants across 222 studies found that the use of video laryngoscopes of one or more designs i.e., Macintoshâstyle video laryngoscopy, hyper angulated video laryngoscopy and channeled video laryngoscopy compared to direct laryngoscopy (DL) reduced the number of failed intubations, particularly in cases with a difficult airway. They improved the view of the glottic aperture and may lead to reduced trauma to peri laryngeal structures. The main finding of the above-mentioned Cochrane review was that the use of video laryngoscopy makes intubation in adults easier, reduces the chances of hypoxemic events, decreased rates of oesophageal intubation and has a better safety profile compared to DL.23
When face mask ventilation is effective but three unsuccessful attempts at intubation of the trachea using direct /video laryngoscopy have been undertaken, the next step to be considered is either awakening the patient, use of a supraglottic airway device (temporizing measure or proceeding), or using a device like a flexible bronchoscope to take a final attempt at intubation of the trachea or ultimately using front-of-neck airway Access (FONA).6,7,8,11
Difficult supraglottic airway (SGA) device insertion
SGAs have ushered in a new era in the management of difficult airway. They can be used as a rescue device and also as a channel for the insertion of the endotracheal tube. They provide a minimally traumatic and less invasive means to secure the airway. Newer features like nasogastric tubes, optimal sealing pressures, integrated bite blocks, and reduced risk of pulmonary aspiration, have established their integral role in difficult airway management.24
Several case reports and case series enumerate the use of SGAs as a means of rescue ventilation when conventional methods of tracheal intubation have failed.25-28 Various observational studies on intubating laryngeal mask airways (ILMA) have reported an intubation success rate of 71.4–100% in patients with difficult airways.28-30
The presence of residual exophytic tumor mass renders insertion of SGA difficult and also predisposes to bleeding.21 Moreover, lack of mandibular support leads to easy dislodgement of SGA. The shift of the hyoid bone position and posterosuperior displacement of the tongue post mandibulectomy may also contribute to decreased efficiency of ventilation via SGA in these patients.
Awake tracheal intubation
The principal indication of awake intubation is that there is a high risk of loss of airway resulting in failed oxygenation which is a possibility in patients with residual tumors in the oropharyngeal region or post mandibulectomy. Thorough patient counselling is essential as the patient is sufficiently awake and maintains spontaneous respiration during this process. Adequate topical airway anesthesia and blocking of 3 principal nerves of the upper airway i.e., glossopharyngeal, superior laryngeal, and recurrent laryngeal nerve with or without the use of sedation is the key to performing successful awake intubation.31 However, airway reflexes, response to stimuli, and ventilation may be diminished by a higher depth of sedation. Post-mandibulectomy patients are predisposed to the development of OSA which limits the degree of safe sedation. Commonly used devices for awake intubation include flexible fibreoptic bronchoscopes (FOBs) or video laryngoscopes in select cases.32 There have been various studies that put the limelight on the use of fibreoptic bronchoscopes in difficult airway management and studies have also reported a higher intubation success rate using fibreoptic guidance.33-36
Can’t intubate, can't oxygenate’ (CICO) scenario
If all else fails i.e., failure of intubation and rescue ventilation, emergency front-of-neck access (eFONA) is necessary. Multiple failed attempts to secure the airway and ensure oxygenation by a tracheal tube, supraglottic airway device, and a facemask lead to a can’t intubate, can't oxygenate’ (CICO) scenario. Profound hypoxia during a CICO situation might lead to hypoxic brain damage, cardiac arrest, and even death. More than 25% of all anesthesia-related deaths are attributed to CICO situations. eFONA is the final and most critical step in the management of such a scenario. Surgical tracheostomy, scalpel cricothyroidotomy, and cannula cricothyroidotomy are the three principal techniques of securing the airway in a CICO scenario.36,37
Nikhar et al. studied perioperative airway management of 156 patients operated on for oral cancers and found that tracheal intubation via nasal route was the preferred means to secure the airway seen in 62.8% of patients. Tracheostomy was used for securing the airway in 19.2% of patients. They also found additional airway techniques like gum elastic bougies (23.6%), McCoy laryngoscopes (13.4%), fibreoptic bronchoscopes (0.03%), and Airtraq devices (0.006%).5
In cases with advanced head and neck cancers or post mandibulectomy with bulky flap reconstruction, conventional techniques of intubation using direct/video laryngoscope seem to have a very high likelihood of failure, and alternative approaches like awake intubation using flexible bronchoscope may not always be possible necessitating a tracheostomy or cricothyroidotomy under local anesthesia with or without sedation as the primary means of securing the airway.13,14
Lin et al. conducted a retrospective analysis of 121 patients who underwent maxillectomies and found only 10 tracheostomies (7.7%) were performed. Four of these tracheostomies were done in patients with bulky flap reconstruction and three in patients undergoing both mandibulectomy and flap reconstruction. They recommended the selective use of tracheostomy to secure the airway during the aforementioned procedures due to the risk of postoperative oropharyngeal airway obstruction.37
Tracheal extubation
Tracheal extubation is always a planned elective procedure. Risk factors like oropharyngeal muscle weakness leading to tongue prolapse, anatomical airway obstruction secondary to airway edema or bulky flap, and cardiopulmonary issues along with compromised functional residual capacity predispose to failure of extubation. It is recommended to use an airway exchange catheter during extubation of a patient in whom reintubation might be difficult post mandibulectomy. For a smooth successful extubation, the patient should be fully awake, following commands, hemodynamically stable with intact cough, gag, and swallowing reflexes, and generate adequate tidal volume.38,39
Follow-up
The anesthesiologist should ensure appropriate documentation of the presence and nature of the airway difficulty and the airway management techniques used to guide and facilitate future care. A follow-up visit to the patient for the evaluation of potential complications of management of the difficult airway like bleeding, airway edema, tracheal/esophageal perforation, pulmonary aspiration, pneumothorax, and subcutaneous emphysema should also be done.7
Conclusion
The various anatomical and physiological changes post mandibulectomy lead to an anticipated difficult airway that can develop into a life-threatening emergency in the absence of careful assessment, extensive preparation, and critical decision-making. In case of failure of the primary attempt at securing the airway, an organized plan outlining the alternative approaches and addressing the reasons for failure is essential. A multidisciplinary team approach, anticipation of complications, and due vigilance can minimize perioperative adverse events leading to the successful management of a difficult airway.
References
- Santagata M, Tozzi U, Lamart E, et al. Effect of Orthognathic Surgery on the Posterior Airway Space in Patients Affected by Skeletal Class III Malocclusion. J Maxillofac Oral Surg. 2015; 14: 682-686.
- Tselnik M, Pogrel MA. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000; 58: 282-285.
- Wickwire NA, White RP Jr, Proffit WR. The effect of mandibular osteotomy on tongue position. J Oral Surg. 1972; 30: 184-90.
- Panje WR, Holmes DK. Mandibulectomy without reconstruction causes sleep apnea. Laryngoscope. 1984; 94: 1591-1594.
- Nikhar SA, Sharma A, Ramdaspally M, et al. Airway Management of Patients Undergoing Oral Cancer Surgery: A Retrospective Analysis of 156 Patients. Turk J Anaesthesiol Reanim. 2017; 45: 108-111.
- Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society intubation guidelines working group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015; 115: 827-48.
- Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for management of the difficult airway. Anesthesiology. 2021; 136: 31-81.
- Law JA, Duggan LV, Asselin M, et al. Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway: Part 1. difficult airway management encountered in an unconscious patient. Can J Anaesth. 2021; 68: 1373-404.
- Kheterpal S, Han R, Tremper KK, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006; 105: 885-91.
- Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology 2000; 92: 1229-36.
- Levitan RM, Heitz JW, Sweeney M, et al. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011; 57: 240-7.
- Heidegger T. Management of the Difficult Airway. N Engl J Med. 2021; 384: 1836-1847.
- Berardi R, Torniai M, Lenci E, et al. Electrolyte disorders in cancer patients: a systematic review. Journal of Cancer Metastasis and Treatment. 2019; 5: 79.
- Anjum Ahmed-Nusrath, FRCA. Anaesthesia for head and neck cancer surgery. BJA Education. 2017; 17: 383-389.
- Johnson KN, Botros DB, Groban L, et al. Anatomic and physiopathologic changes affecting the airway of the elderly patient: implications for geriatric-focused airway management. Clin Interv Aging. 2015; 10: 1925-34.
- Roth D, Pace NL, Lee A, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database of Systematic Reviews. 2018. Art No: CD008874.
- Gomes SH, Simões AM, Nunes AM, et al. Useful ultrasonographic parameters to predict difficult laryngoscopy and difficult tracheal intubation—a systematic review and meta-analysis. Frontiers in Medicine. 2021; 8: 658-671.
- Fernandez-Vaquero MA, Charco-Mora P, Garcia-Aroca MA, et al. Preoperative airway ultrasound assessment in the sniffing position: a prospective observational study. Braz J Anesthesiol. 2022: S0104-0014(22)00088-4.
- Bjurström MF, Bodelsson M, Sturesson LW. The Difficult Airway Trolley: A Narrative Review and Practical Guide. Anesthesiol Res Pract. 2019; 2019: 6780254.
- Fagbohun OA, Dennar I, Sope O, et al. Anaesthesia for Reconstruction Surgery Post Mandibulectomy in a Patient with a Predicted Difficult Airway: A Case Report. Integr J Med Sci. 2021; 24: 8.
- Bradley WPL, Lyons C. Facemask ventilation. BJA Educ. 2022; 22: 5-11.
- Hasegawa K, Shigemitsu K, Hagiwara Y, et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Annals of Emergency Medicine. 2012; 60: 749-754.
- Hansel J, Rogers AM, Lewis SR, et al. Video laryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database of Systematic Reviews. 2022; 4: CD011136.
- Tim Cook FRCA, Ben Howes FRCA. Supraglottic airway devices: recent advances. Continuing Education in Anaesthesia Critical Care & Pain. 2011; 11: 56-61.
- Augoustides JG, Groff BE, Mann DG, et al. Difficult airway management after carotid endarterectomy: utility and limitations of the Laryngeal Mask Airway. J Clin Anesth. 2007; 19: 218-221.
- Fundingsland BW, Benumof JL. Difficulty using a laryngeal mask airway in a patient with lingual tonsil hyperplasia. Anesthesiology. 1996; 84: 1265-6.
- Kidani DC, Shah NK. The use of a laryngeal mask airway after a prolonged suspension laryngoscopy to preserve a vocal cord fat graft. Anesth Analg. 2007; 105: 1753-4.
- Parmet JL, Colonna-Romano P, Horrow JC, et al. The laryngeal mask airway reliably provides rescue ventilation in cases of unanticipated difficult tracheal intubation along with difficult mask ventilation. Anesth Analg. 1998; 87: 661-5.
- Frappier J, Guenoun T, Journois D, et al. Airway management using the intubating laryngeal mask airway for the morbidly obese patient. Anesth Analg. 2003; 96: 1510-596.
- Fukutome T, Amaha K, Nakazawa K, et al. Tracheal intubation through the intubating laryngeal mask airway (LMA-Fastrach) in patients with difficult airways. Anaesth Intensive Care. 1998; 26: 387-91.
- Kapila A, Addy EV, Verghese C, et al. The intubating laryngeal mask airway: An initial assessment of performance. Br J Anaesth. 1997; 79: 710-3.
- Ramkumar V. Preparation of the patient and the airway for awake intubation. Indian J Anaesth. 2011; 55: 442-447.
- Ahmad I, ElâBoghdadly K, Bhagrath R, et al. Difficult airway society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2019; 75: 509-28.
- Wong J, Lee JSE, Wong TGL, et al. Fibreoptic intubation in airway management: A review article. Singapore Medical Journal. 2019; 60: 110-8.
- Collins SR, Blank RS. Fiberoptic intubation: An overview and update. Respiratory Care. 2014; 59: 865-80.
- Price TM, McCoy EP. Emergency front-of-neck access in airway management. BJA Educ. 2019; 19: 246-253.
- Lin HS, Wang D, Fee WE, et al. Airway Management After Maxillectomy: Routine Tracheostomy Is Unnecessary. The Laryngoscope. 2003; 113: 929-932.
- Parotto M, Cooper RM, Behringer EC. Extubation of the Challenging or Difficult Airway. Curr Anesthesiol Rep. 2020; 10: 334-340.
- Kundra P, Garg R, Patwa A, et al. All India Difficult Airway Association 2016 guidelines for the management of anticipated difficult extubation. Indian J Anaesth. 2016; 60: 915-921.
